Managing Treatment-Resistant Depression: Tips for the Outpatient Psychiatrist
Here's how embracing a comprehensive, patient-centered approach and staying informed about emerging treatments can help mental health professionals make a difference in the lives of patients with TRD.
StockPhotoPro_AdobeStoc

SPECIAL REPORT: TREATMENT-RESISTANT DEPRESSION
The management of depression, particularly in the postpandemic era, presents a complex and often challenging endeavor for mental health professionals. Although many individuals with depression respond well to standard treatments, a significant number of patients experience treatment-resistant depression (TRD), requiring revised and innovative approaches and a nuanced understanding of the condition.1
The estimated 12-month prevalence of medication-treated major depressive disorder (MDD) in the United States was 8.9 million adults, and 2.8 million had TRD.2 Clinicians working with patients with TRD should adopt a comprehensive approach, encompassing a thorough understanding of past treatments, the possible role of interventional therapeutic modalities, and the importance of a patient-centered approach.
A Patient-Centered Approach
A critical aspect of treating TRD is adopting a patient-centered approach. Patients often feel frustrated, hopeless, and stigmatized due to their lack of response to conventional treatments. Patients may also perceive their poor response as personal failure.3 To best support success, clinicians must prioritize empathetic, collaborative care that empowers patients and fosters a sense of agency in their recovery (Table 1).
Table 1. The Patient-Centered Approach

Understanding TRD
TRD is typically defined as a failure to respond to 2 or more trials of antidepressant medications at adequate dose and duration.4 However, controversies surround this definition, primarily regarding its perceived incompleteness. Critics argue that it fails to encompass the consideration of alternative treatment modalities, such as neuromodulation techniques and various forms of psychotherapy, potentially overlooking effective interventions for individuals with TRD.
From the STAR*D clinical trial, it is estimated that approximately one-third of individuals with MDD do not achieve remission with initial treatment, and a significant proportion of those patients may go on to develop TRD.1 It manifests in various forms, including partial response, nonresponse, or recurrent depression, despite adequate treatment trials.
When evaluating patients with multiple antidepressant trials and nonresponse, it is important to understand the treatment history. The Antidepressant Treatment Response Questionnaire is a tool that can be useful in the assessment of patients with TRD.
Factors Contributing to Resistance
Before implementing treatment strategies, clinicians must thoroughly assess the factors contributing to presentation of depression in each patient. The limitations of medications targeting monoamines have been acknowledged, and ongoing research into the etiology of depression has led to the development of newer treatments targeting different receptors. Several factors can influence the resistance to treatment in depression.
Biological factors. Alterations in receptor structure and function can make some individuals less responsive to standard antidepressants. Available genetic testing is often misunderstood by clinicians and patients.5 Psychiatric clinicians should be aware of the limitation of the interpretation of these tests before ordering them and interpreting them with patients.
Lifestyle factors. Poor sleep, inadequate nutrition, and lack of physical activity can exacerbate depressive symptoms and hinder treatment success; tips for assessing and addressing these issues can be found in Table 2.
Table 2. Tips to Assess and Address Exacerbating Factors in Depression
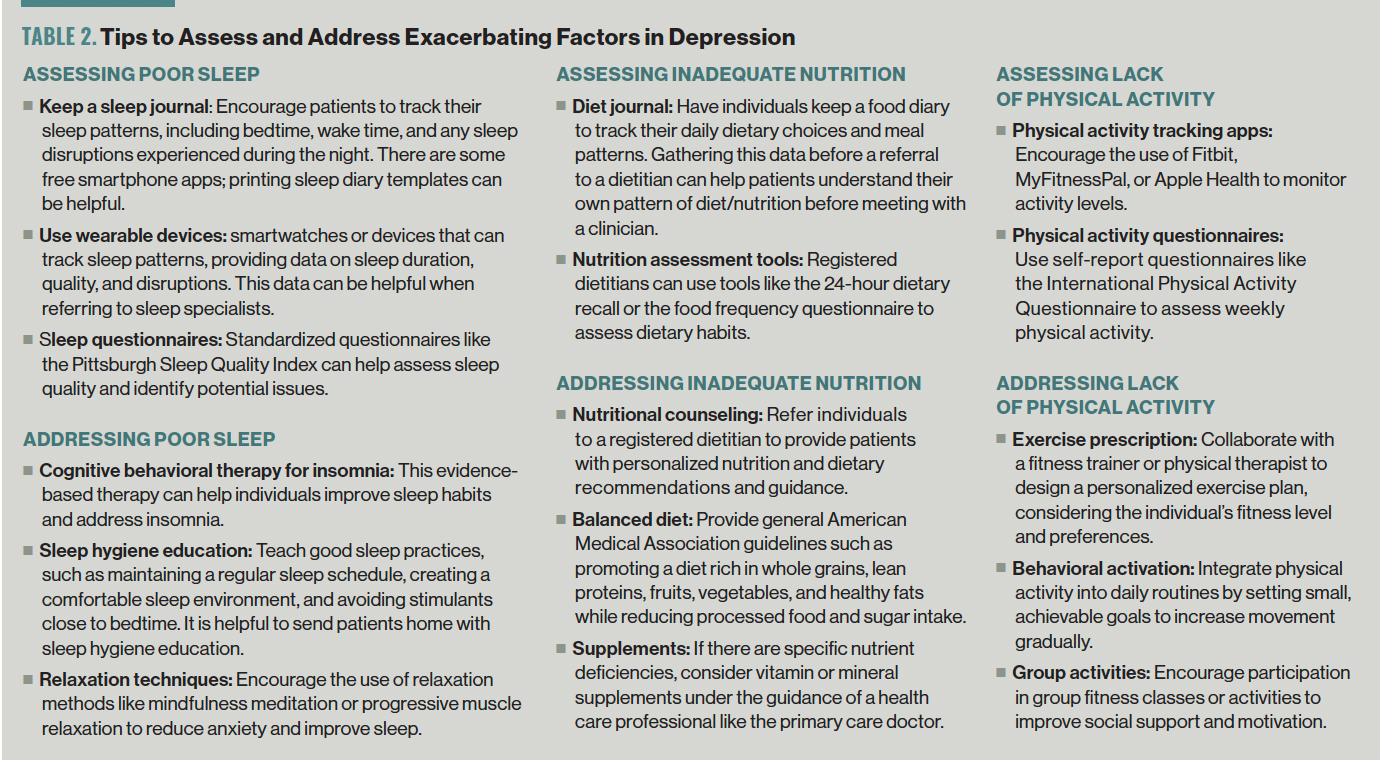
Often, the neurovegetative symptoms of depression need to be given the same level of importance in the overall treatment plan as oral medication.
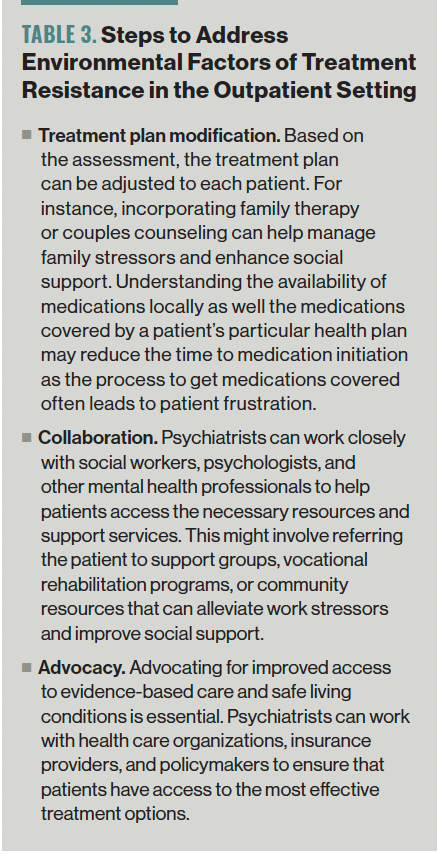
Environmental factors. The lack of social support, family and work stressors, and access to quality mental health care—especially evidence-based psychotherapy and safe living conditions—play crucial roles in treatment resistance. This is, admittedly, a barrier to accessing care that is hard to address without involvement of higher levels of care; however, there are steps clinicians can take to help with tools they have in the outpatient setting (Table 3).
Table 3. Steps to Address Environmental Factors of Treatment Resistance in the Outpatient Setting
Comorbid psychiatric and medical conditions. Comorbid psychiatric conditions, personality traits, and maladaptive coping strategies can complicate treatment outcomes. As an example, clinicians may use assessment tools like the McLean Screening Instrument for Borderline Personality Disorder and the PCL-5 for assessing for comorbid posttraumatic stress disorder.6
The role of psychotherapy in TRD is often not discussed within the definition of TRD but should play an important role.7 The sequelae of chronic substance abuse, untreated diabetes, and chronic pain are examples of comorbid conditions that, if left untreated, are associated with negative outcomes, often exacerbating the physical and psychological aspects of a patient’s well-being.
Optimization Pearls
TRD is a complex condition that demands a multifaceted approach to achieve improvement. Clinicians must consider a range of strategies tailored to each patient’s unique profile. The outpatient setting can offer effective treatment options for patients with TRD.
Comprehensive assessment
Begin with a comprehensive assessment of the patient’s history, including previous treatment trials, medication response, and any potential contributing factors such as substance use or medical conditions.
Having templates and forms that the patient, caregiver, or previous providers can fill out beforehand for review can optimize the face-to-face time spent with the patient. Most electronic health records offer printable forms that can be filled out before appointments. Patient-rated scales that are unlicensed can be added, such as the Beck Depression Inventory and the PHQ-9.8
Medication review
Assess the patient’s medication regimen with a primary focus on determining whether deprescribing could offer benefits. Before contemplating a switch to or augmentation with alternative classes of antidepressants, it is essential to carefully review current guidelines and how they pertain to the patient.9
STAR*D provides some guidance and many peer-reviewed publications offer comprehensive reviews including new treatment options.10 Equally important is to ascertain whether the patient has a clear, realistic understanding of which aspects of their current symptoms antidepressants can effectively address.
Additionally, exploring newer antidepressants that target different receptors may prove beneficial to patients not responding to traditional antidepressants.
Psychotherapy
Commencing psychotherapy should occur when the therapist and the treating clinician collectively determine that the patient is at a point where active participation in therapy is feasible and beneficial. Clinicians employ a comprehensive approach to assess a patient’s suitability for psychotherapy.
There are some rating scales that are used in conjunction with an extensive clinical interview, aimed at gaining insight into the patient’s presenting concerns and personal history. Following this, the clinician evaluates the patient’s motivation and readiness to actively engage in the therapeutic journey, scrutinizing indicators of commitment and a genuine desire for personal growth and change.11
Cognitive-behavioral therapy, dialectical behavior therapy, and interpersonal therapy have demonstrated effectiveness in addressing the challenges of TRD.12,13 These therapeutic modalities offer promising avenues for patients struggling with TRD.
Individualized psychotherapy plays a crucial role in this context, as it enables patients to cultivate essential coping skills, delve into underlying emotional issues, and establish achievable goals for their well-being. In cases in which your practice setting does not provide psychotherapy services, it is advisable to seek out qualified therapists within your geographic area or explore available therapy programs. By doing so, patients can access the specialized support and interventions that can be instrumental in their journey toward managing and eventually overcoming TRD.
Neuromodulation therapies
Noninvasive neuromodulation techniques, such as transcranial magnetic stimulation (TMS) and electroconvulsive therapy (ECT), have shown effectiveness in cases of TRD. More recent comparative studies have provided evidence affirming the efficacy of ECT, despite the enduring negative connotation historically associated with this treatment approach.14
TMS has had notable advancements in recent years, including the US Food and Drug Administration (FDA) approval of the SAINT Neuromodulation System for treating refractory depression in adults.15 However, widespread insurance reimbursement remains elusive, and its impracticality for outpatient settings has led to the emergence of modified treatment variations that deviate from the intended protocol.
Esketamine therapy
Esketamine, an N-methyl-D-aspartate receptor antagonist, has gained FDA approval as a rapid-acting antidepressant. It has also been approved by the FDA for the treatment of depressive symptoms in patients with MDD with acute suicidal ideation. It is administered under medical supervision; intranasal esketamine may provide relief to some patients with TRD where accessibility to this kind of care allows.
A subgroup analysis of the SUSTAIN-3 clinical trial demonstrated that in adults with TRD, improvements in depressive symptoms appear to be maintained up to 6.5 years with long-term treatment.16
Intravenous ketamine
Intravenous ketamine has been used off-label for depression with reported benefits for TRD. However, there is no widespread consensus on its use in psychiatry, and due to its off-label status, access to care remains elusive for many patients, primarily due to the burden of out-of-pocket costs.17
Lifestyle modification. Encouraging patients to embrace healthy lifestyle modifications, such as incorporating regular exercise, maintaining a balanced diet, and enhancing their sleep hygiene, can have a profound influence on mood and overall well-being.
Although it may seem like a substantial endeavor during a typical visit, adopting a targeted approach with incremental information, particularly tailored to specific patient populations, can make a meaningful difference. Encourage patients to explore their health care benefits, as many plans offer incentives for weight loss and offer group support.
Mindfulness and meditation
Mindfulness-based therapies and meditation techniques can help patients manage stress, reduce rumination, and improve emotional regulation, all of which can be beneficial in TRD.18 In fact, in one study at 52 weeks, 48% of patients had a sustained response. Many cities and towns offer free classes or sliding-scale classes.
Supportive care
Ensure that patients have access to a robust support system, which may include family, friends, or support groups. Social isolation can exacerbate depression, so fostering connections is crucial.
Collaboration
Consider consulting with a team of mental health professionals, including colleagues in psychiatry, psychologists, social workers, and occupational therapists. A collaborative approach can provide a more holistic perspective on the patient’s needs.19
Monitoring and follow-up
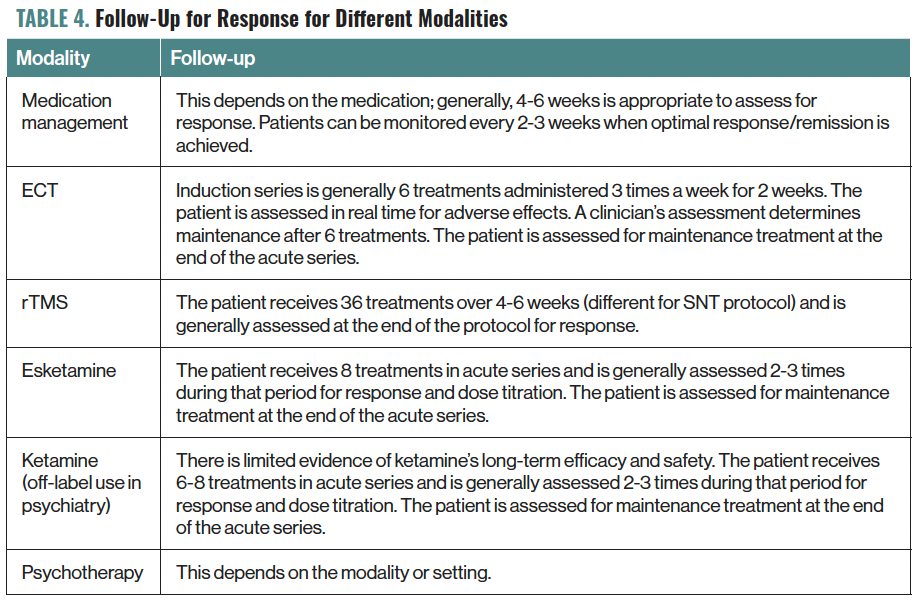
Regularly assess the patient’s progress and adjust treatment plans as needed. Close monitoring can help identify emerging issues and facilitate timely interventions. Patients with TRD need to be monitored as they start new therapies.20 If new medications are started, 4 to 6 weeks is a general guideline to monitor for adverse effects and for response.
When a patient is receiving an intervention (eg, repetitive TMS, esketamine, or ECT), they are monitored during the procedure by clinical staff. Follow-up to assess for response will be procedure specific (Table 4).
Table 4. Follow-Up for Response for Different Modalities
Emerging Treatments and Research
In recent years, continuous research has revealed promising prospects in the treatment of TRD. Psychedelics, although not yet FDA approved, have garnered significant interest, offering potential new hope for patients resistant to conventional treatments. Staying informed about the latest developments is crucial to understanding the limitations of these emerging therapies.
Concluding Thoughts
TRD is a formidable challenge for clinicians, but it is not insurmountable. By embracing a comprehensive, patient-centered approach and staying informed about emerging treatments, mental health professionals can make a significant difference in the lives of individuals struggling with TRD.
Through collaboration, perseverance, and compassion, clinicians can offer hope and the possibility of recovery to those who need it most. As the field of psychiatry evolves, there is reason to believe that even more effective treatments for TRD will emerge, offering new opportunities for healing and relief.
Dr Harding is a board-certified psychiatrist and intervention specialist in Milford, Connecticut.
References
1. Pigott HE. The STAR*D Trial: It is time to reexamine the clinical beliefs that guide the treatment of major depression. Can J Psychiatry. 2015;60(1):9-13.
2. Zhdanava M, Pilon D, Ghelerter I, et al. The prevalence and national burden of treatment-resistant depression and major depressive disorder in the United States. J Clin Psychiatry. 2021;82(2):20m13699.
3. Nelson E, Werremeyer A, Kelly GA, Skoy E. Self-stigma of antidepressant users through secondary analysis of PhotoVoice data. Ment Health Clin. 2018;8(5):214-221.
4. Fava M. Diagnosis and definition of treatment-resistant depression. Biol Psychiatry. 2003;53(8):649-659.
5. Dubovsky SL. The limitations of genetic testing in psychiatry. Psychother Psychosom. 2016;85(3):129-135.
6. Zimmerman M, Balling C. Screening for borderline personality disorder with the McLean Screening Instrument: a review and critique of the literature. J Pers Disord. 2021;35(2):288-298.
7. Markowitz JC, Wright JH, Peeters F, et al. The neglected role of psychotherapy for treatment-resistant depression. Am J Psychiatry. 2022;179(2):90-93.
8. Assessment tools. American Psychological Association. Updated June 2020. Accessed October 12, 2023. https://www.apa.org/pi/about/publications/caregivers/practice-settings/assessment/tools
9. Nuñez NA, Joseph B, Pahwa M, et al. Augmentation strategies for treatment resistant major depression: a systematic review and network meta-analysis. J Affect Disord. 2022;302:385-400.
10. Warner J, Philip NS. Augmentation strategies in MDD therapy. Psychiatric Times. September 10, 2013. https://www.psychiatrictimes.com/view/augmentation-strategies-mdd-therapy
11. Ghomi M, Wrightman M, Ghaemian A, et al. Development and validation of the Readiness for Therapy Questionnaire (RTQ). Behav Cogn Psychother. 2021;49(4):413-425.
12. Munder T, Flückiger C, Leichsenring F, et al. Is psychotherapy effective? A re-analysis of treatments for depression. Epidemiol Psychiatr Sci. 2019;28(3):268-274.
13. van Bronswijk S, Moopen N, Beijers L, et al. Effectiveness of psychotherapy for treatment-resistant depression: a meta-analysis and meta-regression. Psychol Med. 2019;49(3):366-379.
14. Mathew SJ, Wilkinson ST, Altinay M, et al. Electroconvulsive therapy (ECT) vs. ketamine in patients with treatment-resistant depression: the ELEKT-D study protocol. Contemp Clin Trials. 2019;77:19-26.
15. Zagorski N. FDA clears accelerated TMS protocol for depression. Psychiatr News. September 23, 2022. Accessed October 3, 2023. https://psychnews.psychiatryonline.org/doi/full/10.1176/appi.pn.2022.10.10.40
16. Zajecka J, Zaki N, Fu D, et al. Long-term efficacy of esketamine nasal spray dosed in accordance with US prescribing information in adults with treatment-resistant depression: a subgroup analysis of the SUSTAIN-3 study up to 6.5 years. Poster presented at: Psych Congress; September 6-10, 2023; Nashville, TN.
17. Harding L. Regulating ketamine use in psychiatry. J Am Acad Psychiatry Law. 2023;51(3):320-325.
18. Eisendrath SJ, Gillung E, Delucchi KL, et al. A randomized controlled trial of mindfulness-based cognitive therapy for treatment-resistant depression. Psychother Psychosom. 2016;85(2):99-110.
19. Reist C, Petiwala I, Latimer J, et al. Collaborative mental health care: a narrative review. Medicine (Baltimore). 2022;101(52):e32554.
20. Practice guideline for the treatment of patients with major depressive disorder (third edition). American Psychiatric Association. Am J Psychiatry. 2010;167(suppl):1-152.

