CME
Article
Psychiatric Times
Intimate Partner Violence Victimization: How It Relates to Substance Use in Women
Author(s):
In this CME, review the risks and clinical implications of intimate partner violence on women’s substance use and treatment.
doidam10/AdobeStock

CATEGORY 1 CME
Premiere Date: November 20, 2023
Expiration Date: May 20, 2025
This activity offers CE credits for:
1. Physicians (CME)
2. Other
All other clinicians either will receive a CME Attendance Certificate or may choose any of the types of CE credit being offered.
ACTIVITY GOAL
The goal of this activity is to review the risks and clinical implications of intimate partner violence (IPV) on women’s substance use and treatment.
LEARNING OBJECTIVES
After engaging with the content of this CME activity, you should be better prepared to:
• Understand the link between IPV victimization and women’s substance use.
• Reflect on how best to engage these patients and promote recovery.
TARGET AUDIENCE
This accredited continuing education (CE) activity is intended for psychiatrists, psychologists, primary care physicians, physician assistants, nurse practitioners, and other health care professionals who seek to improve their care for patients with mental health disorders.
ACCREDITATION/CREDIT DESIGNATION/FINANCIAL SUPPORT
This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of Physicians’ Education Resource®, LLC, and Psychiatric Times®. Physicians’ Education Resource, LLC, is accredited by the ACCME to provide continuing medical education for physicians.
Physicians’ Education Resource, LLC, designates this enduring material for a maximum of 1.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
This activity is funded entirely by Physicians’ Education Resource, LLC. No commercial support was received.
OFF-LABEL DISCLOSURE/DISCLAIMER
This accredited CE activity may or may not discuss investigational, unapproved, or off-label use of drugs. Participants are advised to consult prescribing information for any products discussed. The information provided in this accredited CE activity is for continuing medical education purposes only and is not meant to substitute for the independent clinical judgment of a physician relative to diagnostic or treatment options for a specific patient’s medical condition. The opinions expressed in the content are solely those of the individual faculty members and do not reflect those of Physicians’ Education Resource, LLC.
FACULTY, STAFF, AND PLANNERS’ DISCLOSURES AND CONFLICT OF INTEREST (COI) MITIGATION
None of the staff of Physicians’ Education Resource, LLC, or Psychiatric Times or the planners of this educational activity have relevant financial relationship(s) to disclose with ineligible companies whose primary business is producing, marketing, selling, reselling, or distributing health care products used by or on patients. Tony P. George, MD, FRCPC, reports that he receives grant/research support from NIDA and CIHR and other support from ACNP and CCSA.
For content-related questions, email us at PTEditor@mmhgroup.com; for questions concerning the accreditation of this CME activity or how to claim credit, please contact info@gotoper.com and include “Intimate Partner Violence Victimization: How It Relates to Substance Use in Women” in the subject line.
HOW TO CLAIM CREDIT
Once you have read the article, please use the following URL to evaluate and request credit: https://education.gotoper.com/activity/ptcme23nov. If you do not already have an account with PER®, you will be prompted to create one. You must have an account to evaluate and request credit for this activity.
The World Health Organization (WHO) describes intimate partner violence (IPV) against women as any behavior by a former or current intimate partner that causes physical, sexual, or psychological harm to the victim.1 IPV involves a recurring pattern of power and control, with periods of abuse and nonabuse.2 IPV is not specific to women or to heterosexual relationships. Nevertheless, women tend to be more susceptible to IPV victimization, with data from US nationwide surveys suggesting that approximately 41% of women experience IPV in their lifetime, in comparison with 26% of men.3 Moreover, in the United States, more than half of female homicides were committed by a current or former male intimate partner.
IPV can appear in multiple forms. The most discussed form is physical violence, or the use of physical force on an individual, leading to injury or harm (eg, scratching, pushing, punching, use of a weapon). Sexual violence refers to sexual acts committed against an intimate partner without consent (eg, sexual assault, coercion, forced consumption of pornography, reproductive abuse). Psychological aggression intends to control an individual and/or harm them mentally or emotionally.4 Both expressive aggression (eg, humiliation, threats, gaslighting) and coercive control over a partner’s life (eg, monitoring partners’ relationships, using blackmail) fall under psychological IPV. A notable example of coercive control is financial abuse, whereby a partner controls money or limits the woman’s ability to earn money through work.5 This financial control can impact how prepared a woman feels to leave a situation with an abusive partner.
Who Is at Greater Risk for IPV?
There are several populations who are more vulnerable to IPV than others. Pregnant women are at greater risk for IPV, leading to negative consequences for children, with IPV being associated with low birth weight and preterm birth due to the effects of maternal stress.6 Marginalized communities, including older women, women with disabilities, and ethnic minorities, may be disproportionately impacted by IPV.7 Research examining transgender individuals’ experiences of IPV found that both female-to-male and male-to-female transgender individuals are 1.7 times more likely to experience IPV than both cisgender straight and cisgender sexual minority individuals.8
Furthermore, women of color (WOC) are more susceptible to recurrent IPV and more likely to experience lower socioeconomic status than White women, further exacerbating existing challenges to accessing formal supports for their IPV.2,9 Due to the stigma associated with IPV and increased cultural pressure to maintain a good family reputation, WOC are also less likely than Caucasian women to seek treatment.9 Factors related to cultural expectations (eg, stereotypes, gender roles, etc) and immigration status remain barriers to these populations who are seeking help.2
IPV has also been further exacerbated by the COVID-19 pandemic. Increased household stress, job loss, and isolation from support systems can impact whether or not IPV occurs. Additionally, there are fewer opportunities for women to access help, including (but not limited to) sexual/reproductive health services, shelters, crisis centers, and protection services.7
IPV and Trauma
According to research findings, 31% to 84% of women experiencing IPV further develop posttraumatic stress disorder (PTSD). PTSD remains the most prevalent mental health disorder in IPV survivors, with common symptoms listed in Table 1.10 Moreover, women who experience lifetime IPV report more physical symptoms and poorer health status than nonexposed individuals. These psychological and health issues are further exacerbated by the severity of the violence.10
Table 1. Common Symptoms of PTSD10
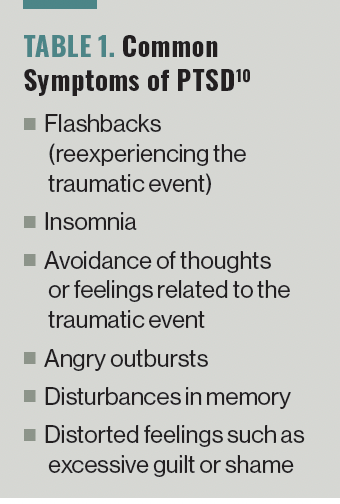
Even without a formal diagnosis, trauma can impact an individual’s functioning. Women who do not meet all the diagnostic criteria for PTSD still experience clinically significant levels of functional impairment.11 Women experiencing IPV also face an increased health burden and higher risk for chronic disease.12 Potential health behavior pathways to negative health outcomes through trauma may involve medical treatment nonadherence and poorer coping strategies for dealing with trauma, such as substance use. However, it is challenging to identify specific effects of different traumas, as many studies either entirely neglect nonphysical forms of IPV or do not distinguish between different forms of IPV, including psychological/verbal, physical, and sexual violence.13
Substance Use as a Coping Mechanism for IPV
The experience of substance use in women differs from that of men. Biological factors such as estradiol levels, stress reactivity, and sexual differences in brain structures may impact substance use. Co-occurring mental health disorders including major depression, anxiety, PTSD, and eating disorders are more prevalent in women than in men. Further, greater stigma is associated with substance use in women, in whom the behavior is considered “deviant” because of the role of the woman in the family and in society (eg, as a mother).14 This further creates barriers for women to access treatment for their substance use.
Moreover, IPV tends to be chronic, and its effects can have long-term consequences on women’s experiences of psychological stress (Table 2).15 This can lead to poor decision-making, memorization and concentration problems, behavioral responses to pain, and mental health challenges (eg, depression, anxiety).
Table 2. Long-Term Consequences of Chronic IPV on Women’s Psychological Stress15

There is a relationship between women’s substance use and co-occurring IPV in which increased rates of substance use disorders (SUDs) are directly correlated with increased prevalence of IPV.13 Approximately 90% of women with SUD report lifetime experiences of psychological abuse, and up to 71% report emotional abuse in the past year.5 Similarly, physical and sexual abuse have been found to be related to higher rates of alcohol and other substance use.16 Women using crack, cocaine, and heroin were also twice as likely to experience later IPV in the next 6 months.17
Tranquilizers, prescription drugs, and nonprescription drugs are the most common substances of choice for victims. Drug use is common in both the perpetrator and the victim. Often, women who experience IPV cope with their experiences through the use of substances, wishing to feel numb or to feel good when using the substance.5 The literature suggests a bidirectional relationship between women’s substance use and IPV, highlighting the complexity of this issue.17
Impacts of IPV on Women’s Substance Use Treatment Outcomes
As trauma can contribute to increased substance use, higher chance of relapse, and greater likelihood of experiencing a co-occurring mental illness,18 it is unsurprising that increased substance use behaviors, including relapse, were observed in women with SUD when they were experiencing IPV.5 Severity of anxiety and PTSD symptomatology have been found to be affiliated with alcohol and drug problems in women who are victims of IPV.19
Additionally, evidence has shown that women experiencing IPV at treatment entry were less likely to complete treatment and had a lower likelihood of achieving abstinence after a 12-month follow-up,13,16 with emotional and financial abuse having been cited as a barrier to engagement in substance use treatments.5
Case Study
“Caroline” was raised in a low-income neighborhood by a single mother who had various partners she would bring home. She started to drink alcohol and use cannabis at age 15 years, with increasing frequency as she got older.
At the age of 18 years, Caroline moved out of her mother’s house to live with her 25-year-old boyfriend, whom she met at a bar. She thought this would be better for her because her partner seemed to be kind and respectful. After 5 months of living together, her boyfriend’s expectations of what she should be doing in and around the house began to change. He began to exhibit behaviors of coercive control, forcing her to dress in a certain way and taking her paychecks. Simultaneously, he began verbally abusing her, making negative statements about her appearance and undermining her self-worth.
Under financial and emotional stress, Caroline started to drink considerable amounts of alcohol to cope with these challenges. Upon discovering that she was pregnant, Caroline visited her primary care physician to discuss future steps, which created an opportunity for her IPV to be addressed.
How Do We Treat IPV?
To better respond to IPV in patient populations, there must be frameworks in place at both the structural and the organizational levels. Structural supports, including IPV policies, IPV response protocols, financial resources to support these protocols, and coordination of initiatives, allow for better support for organizations to deliver effective care with educated, motivated, and confident staff.20
Compared with sequential and parallel (eg, simultaneous but not coordinated) treatment, integrated approaches combining substance use and mental illness treatment has greater efficacy for women experiencing IPV.21 Thus, for women who struggle with substance use and IPV, integration of gender-responsive, trauma-informed mental health care is imperative. This involves integration of IPV and substance use treatment; collaboration between mental health and addiction services; and the creation of safe spaces within clinician settings.18
When integration is not possible, highly coordinated service delivery with cross-training of staff in both IPV and substance use can be useful.17 Typically, women are referred to substance use treatment through pathways involving domestic violence shelters or other mental health services.22 Institutions should work to ensure that clinicians can provide a confidential first-line response and establish a protocol for handling these cases with a standard referral pathway in place.23 Barriers to integrating components addressing IPV in substance use treatments include philosophical ideologies and orientations, service delivery models, funding mechanisms, and desired treatment outcomes.17
On top of this integrated approach to substance use, additional resources are required to best serve these patients. Psychological therapies alone are unable to address outcomes related to quality of life, access to and engagement in health care/IPV services, or reexposure to IPV. Clinicians need to offer strategies consistent with individualized goals that are trauma informed and that advocate for the patient. This typically means working in an interdisciplinary team or also seeking training to promote safety and recovery for female victims of IPV. Patient-centered approaches to care are needed to ensure that women feel safe enough to engage in treatment.22
Building specific skills such as empathetic listening and the ability to refer to other services within the community are beneficial and can greatly impact recovery.20 Sensitivity to situations in which women are coming from shelters or other services can make a difference in a woman’s comfort and trust in the clinician.22
Overall, it would be beneficial if service providers were able to receive training in identifying signs of IPV.9 It has been found that physicians who have been trained to respond to IPV in residency or after licensing are better able to identify IPV victims through routine questioning.23 Additionally, clinicians should be able to identify other health matters, notably neurological or neuropsychological damage, especially since 90% of physical injuries in abused women are found on the head, face, or neck regions.15
It is also important to ensure that clinicians are equipped with the correct attitudes and behaviors when they interact with women about this sensitive topic.23 When treating WOC, it is important for service providers to avoid stereotyping and labeling, as these can act as further barriers to treatment in a vulnerable population. Mandatory cultural competency training can help encourage greater awareness of biases against WOC and IPV survivors. Promotion of culturally competent care can also assist in tackling the mistrust that WOC feel toward service providers.9
Revisiting the Case Study
Caroline’s visit to her primary care physician for alternate reasons allowed for the opportunity for her IPV to be identified with a properly trained physician. It would be beneficial not only to provide treatment options for her substance use but to address her mental and financial challenges. In addition to treatment for her drinking, a therapist trained to handle trauma may be beneficial to her recovery. A social worker may be best equipped to assist with access to other resources such as financial advising, job services, and affordable housing, should Caroline choose to leave her boyfriend.
Concluding Thoughts
Clearly, an interdisciplinary approach would greatly benefit women who are experiencing IPV. Substance use linked to IPV is a complex health issue that must be addressed with a diversity of integrated services to best treat those who are in similar situations to Caroline.
Ms Dela Cruz is a research analyst at the Centre for Addiction and Mental Health (CAMH) in Toronto, Canada, and is a graduate of the Institute of Medical Science at the University of Toronto. Ms Zhang is a master’s degree student and Ms Sorkhou is a PhD student at the Institute of Medical Science at the University of Toronto. Ms Praecht is a master’s degree student in neurosciences at the University of Heidelberg in Germany. Dr George is a professor of psychiatry at the University of Toronto and a clinician-scientist at CAMH. He is also a member of the Editorial Board of Psychiatric Times and co-principal editor of Neuropsychopharmacology, the official journal of the American College of Neuropsychopharmacology.
References
1. Violence against women prevalence estimates, 2018: global, regional and national prevalence estimates for intimate partner violence against women and global and regional prevalence estimates for non-partner sexual violence against women. World Health Organization. 2021. Accessed March 1, 2023. https://apps.who.int/iris/handle/10665/341337
2. Alvarez C, Lameiras-Fernandez M, Holliday CN, et al. Latina and Caribbean immigrant women’s experiences with intimate partner violence: a story of ambivalent sexism. J Interpers Violence. 2021;36(7-8):3831-3854.
3. Fast facts: preventing intimate partner violence. CDC. Updated October 11, 2022. Accessed March 1, 2023. https://www.cdc.gov/violenceprevention/intimatepartnerviolence/fastfact.html
4. Breiding MJ, Basile KC, Smith SG, et al. Intimate Partner Violence Surveillance: Uniform Definitions and Recommended Data Elements. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2015.
5. Pallatino C, Chang JC, Krans EE. The intersection of intimate partner violence and substance use among women with opioid use disorder. Subst Abus. 2021;42(2):197-204.
6. Hill A, Pallitto C, McCleary-Sills J, García-Moreno C. A systematic review and meta-analysis of intimate partner violence during pregnancy and selected birth outcomes. Int J Gynaecol Obstet. 2016;133(3):269-276.
7. Roesch E, Amin A, Gupta J, García-Moreno C. Violence against women during Covid-19 pandemic restrictions. BMJ. 2020;369:m1712.
8. Peitzmeier SM, Malik M, Kattari SK, et al. Intimate partner violence in transgender populations: systematic review and meta-analysis of prevalence and correlates. Am J Public Health. 2020;110(9):e1-e14.
9. Bent-Goodley TB. Health disparities and violence against women: why and how cultural and societal influences matter. Trauma Violence Abuse. 2007;8(2):90-104.
10. Fernández-Fillol C, Pitsiakou C, Perez-Garcia M, et al. Complex PTSD in survivors of intimate partner violence: risk factors related to symptoms and diagnoses. Eur J Psychotraumatol. 2021;12(1):2003616.
11. Simpson TL, Hawrilenko M, Goldberg S, et al. Treatment receipt patterns among individuals with co-occurring posttraumatic stress disorder (PTSD) and substance use disorders. J Consult Clin Psychol. 2020;88(11):1039-1051.
12. Mathew A, Smith LS, Marsh B, Houry D. Relationship of intimate partner violence to health status, chronic disease, and screening behaviors. J Interpers Violence. 2013;28(12):2581-2592.
13. Ogden SN, Dichter ME, Bazzi AR. Intimate partner violence as a predictor of substance use outcomes among women: a systematic review. Addict Behav. 2022;127:107214.
14. Fonseca F, Robles-Martínez M, Tirado-Muñoz J, et al. A gender perspective of addictive disorders. Curr Addict Rep. 2021;8(1):89-99.
15. Wong JYH, Fong DYT, Lai V, Tiwari A. Bridging intimate partner violence and the human brain: a literature review. Trauma Violence Abuse. 2014;15(1):22-33.
16. Haro B, López-Goñi JJ, Fernández-Montalvo J, Arteaga A. Prevalence and differential profile of patients with substance use disorder who have suffered physical and/or sexual abuse. J Interpers Violence. 2022;37(15-16):NP12820-NP12837.
17. Mason R, Du Mont J. Advancing our knowledge of the complexity and management of intimate partner violence and co-occurring mental health and substance abuse problems in women. F1000Prime Rep. 2015;7:65.
18. Johnstone S, Dela Cruz GA, Kalb N, et al. A systematic review of gender-responsive and integrated substance use disorder treatment programs for women with co-occurring disorders. Am J Drug Alcohol Abuse. 2023;49(1):21-42.
19. Jaquier V, Flanagan JC, Sullivan TP. Anxiety and posttraumatic stress symptom pathways to substance use problems among community women experiencing intimate partner violence. Anxiety Stress Coping. 2015;28(4):445-455.
20. Colombini M, Mayhew SH, García-Moreno C, et al. Improving health system readiness to address violence against women and girls: a conceptual framework. BMC Health Serv Res. 2022;22(1):1429.
21. McKee SA, Hilton NZ. Co-occurring substance use, PTSD, and IPV victimization: implications for female offender services. Trauma Violence Abuse. 2019;20(3):303-314.
22. Hameed M, O’Doherty L, Gilchrist G, et al. Psychological therapies for women who experience intimate partner violence. Cochrane Database Syst Rev. 2020;7(7):CD013017.
23. Kalra N, Hooker L, Reisenhofer S, et al. Training healthcare providers to respond to intimate partner violence against women. Cochrane Database Syst Rev. 2021;5(5):CD012423.
Newsletter
Receive trusted psychiatric news, expert analysis, and clinical insights — subscribe today to support your practice and your patients.






