How to Effectively Prescribe Exercise
Exercise can be a useful tool in managing symptoms of anxiety and depression. Learn how you can integrate exercise prescriptions into your treatment plans.
onephoto/AdobeStock

Over the past few decades, the level of sedentariness has increased and become a leading public health concern. Greater total sedentary time and longer sedentary bouts are associated with higher all-cause mortality risk.1 This is of even greater concern during the coronavirus 19 (COVID-19) pandemic, as the work force has changed dramatically with various institutions attempting to maintain their workers remotely.
The access to recreation centers and fitness facilities has decreased significantly for public safety purposes. This has made it particularly difficult to advise patients on how to pursue exercise. Yet, in psychiatry, we all prescribe exercise as a natural therapy to improve mood and manage depression and anxiety symptoms. There is a large body of evidence to suggest its benefits.2
While most of us appreciate its importance, we also recognize that avoidance is exceedingly common. Too often patients hear the word exercise and develop an aversive reaction, as they anticipate that it involves intensive training reserved only for the athletically elite. So how can one simply and effectively counsel a patient on exercise to increase their chances of engagement?
The fact that exercise should be part of the treatment regimen for depression seems to be common knowledge, but it is important to emphasize studies from which this insight was formed. A large study of over 30,000 participants showed that 1 hour or more of exercise per week can prevent 12% of future cases of depression.3 Furthermore, 30 minutes of exercise on a stationary bike reduced depression symptoms 10 and 30 minutes post-exercise.4 Fascinatingly, these results are independent of the intensity of exercise.
While exercise has been reported to prevent depression and combat symptoms acutely, it has also been found to improve long term remission rates. One study found a reduction in depressive symptoms by 47% after 12 weeks of regular exercise.5 Another study showed that home-based exercise or supervised exercise resulted in statistically similar remission rates of major depressive disorder (MDD) as selective serotonin reuptake inhibitor (SSRI) use, albeit the sample size consisted more of those with mild depressive symptomatology.6 Even a year after study completion, the remission rates were correlated with the amount of regular exercise, with protective effects maximized at 180 minutes per week.7
While the above studies focused primarily on aerobic physical activity, strength and resistance training can provide similar reductions in depression symptoms. A large meta-analysis of 33 randomized controlled trials showed that regular resistance training significantly reduced symptoms of depression.8 There is substantial improvement in mood by combining both aerobic physical activity and strength training.9,10 Strength training can reduce depression symptoms by 2 to 3 times that of the control group while also reducing bodily pain and improving vitality and social functioning.11 Furthermore, it is important to prevent obesity as it is strongly linked to increasing anxiety symptoms.12 Indeed, it is clear that regular exercise, both aerobic and strength training, can reduce the risk of developing depression, treat depression symptoms acutely, and provide long-term remission.
The exercise programs used in the aforementioned studies often included cycling on a stationary bike or the use of a treadmill. The participants used the bike or treadmill for 30 to 45 minutes4-6,9 with 1 study requiring the heart rate to achieve 75% to 85% of maximum heart rate reserve.6 Other studies simply relied on patients self-reporting weekly exercise, which included activities such as walking and swimming.3,10 Strength training regimens targeted large muscle groups and included exercises such as chest press, lat pulldown, leg press, leg extension, and knee flexion 2 to 3 times per week.9,11 Regardless of the type of physical activity, all exercise sessions lasted 45 minutes or less. Results were often intensity independent, suggesting that even 30 to 45 minutes of mild to moderate intensity exercise a few days a week is sufficient to improve mood symptoms.
While there is strong evidence that regular exercise can improve one’s mood, the clinician must prescribe exercise in a way that promotes adherence. Practical strategies include being specific with exercise routines, but also to listen to the patient’s preferences and barriers to exercise. These strategies will help formulate a program that the patient can maintain.13 It is also helpful to construct goal-oriented objectives that a patient can successfully achieve.13 In addition, it is beneficial to break larger exercise requirements into smaller, achievable chunks. Finding motivation is crucial, which can be done through strategies such as stressing the mood elevating properties of exercise or by encouraging social workouts. It has been shown that those who exercise with others more or equally as often than alone report greater self-health.14
After condensing the information in the literature and combing it with strategies for compliance, we feel it is possible to come up with sample exercise prescriptions. For example, a patient with low exercise tolerance and motivation could be prescribed 30 minutes of moderate walking. The patient could start by walking 1 to 2 days a week and gradually increase to up to 6 days, which would equate to 180 minutes per week. If the patient is having a particularly hard time with motivation, the clinician can encourage walking with a friend and setting goals. In a patient who is aversive to aerobic activity, the clinician can prescribe strength and resistance training that focuses on large muscle groups. These strength sessions can be prescribed 2 to 3 times per week and up to 45 minutes per session. Exercises should target large muscle groups and include activities such as chest press, lat pulldown, leg press, leg extension, and knee flexion. If a patient does not have access to a fitness center or prefers home workouts, then they can perform exercises at home such as push-ups, air squats, wall-sits, and abdominal routines. Since the mood benefits of exercise have often been shown to be intensity independent, it is more than possible to work within the patient’s exercise tolerance and physical limits.
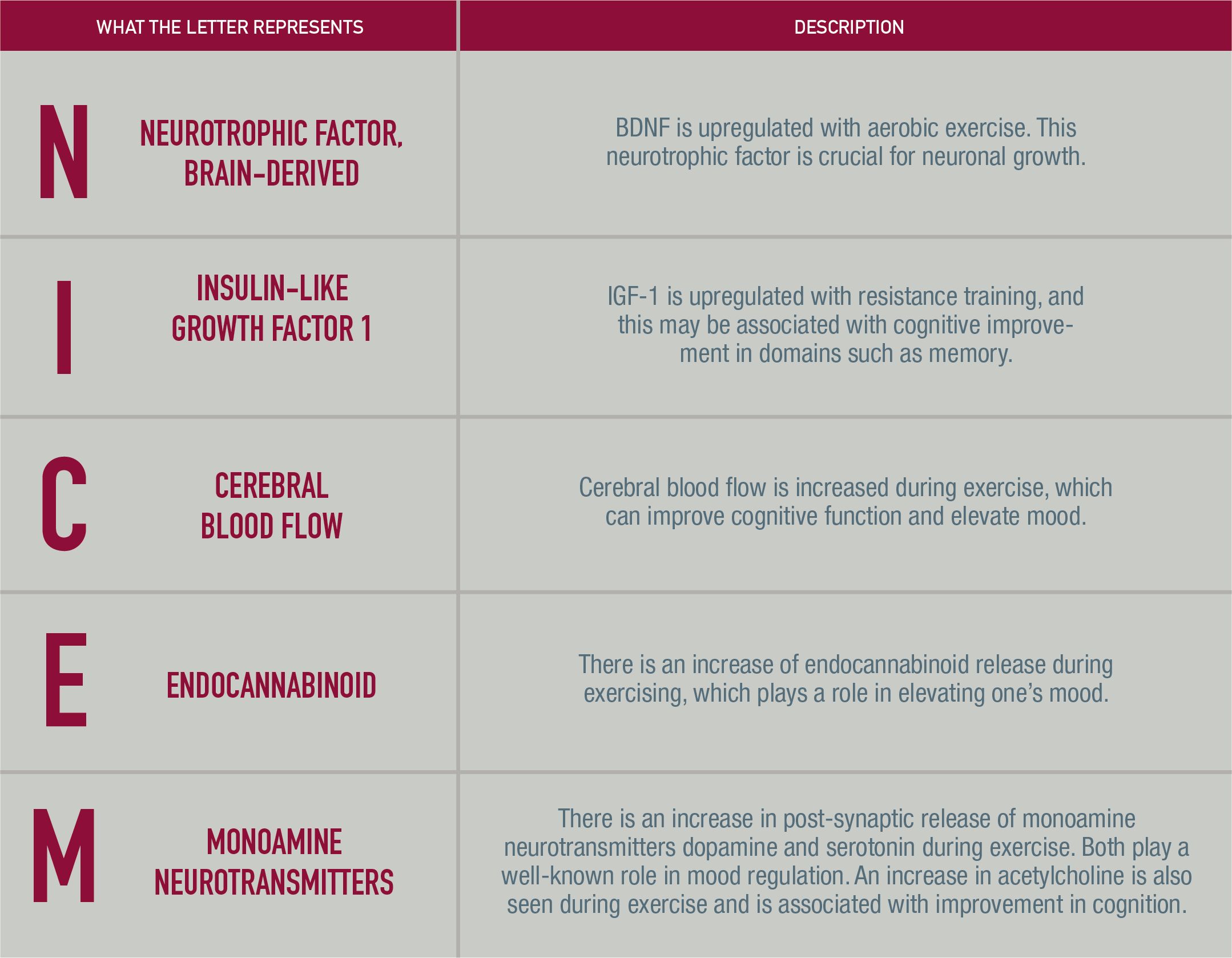
In addition, it can be beneficial to discuss with patients the neurobiological changes seen during exercise that may contribute to elevation of mood and improved cognition. Aerobic fitness is associated with greater hippocampal volume and memory performance.15 Exercise also increases performance in the area of executive functioning, which is attributed to greater function of the anterior cingulate and prefrontal cortices.16 Moreover, aerobic exercising upregulates brain-derived neurotrophic factor (BDNF)17 and enhances dopamine18, serotonin19, and acetylcholine neurotransmitter release20, all of which play a role in mood and cognition.
Resistance training has been shown to improve memory performance and verbal concept formation potentially through increased insulin-like growth factor-1 (IGF-1).21 Additionally, exercise training has shown to improve regional cerebral blood flow in sedentary older men.22 Endocannabinoids also play a role, as there is an increase in release during exercise which may contribute to some of the mood elevating effects.23 Certainly reviewing the neurobiological and cognitive alterations seen in exercise may aid in further justifying to the patient that physical activity can be as efficacious as psychopharmacotherapy.
If approaching a formal discussion on exercise is relatively novel for a clinician, they could benefit from the use of the following SPORT mnemonic (Table 1). Furthermore, the NICE monoamine mnemonic (Table 2) can be used to lead the conversation around the neurobiological changes seen during exercise.
Table 1. The SPORT mnemonic shows how a clinician can structure a discussion around exercise to assist in writing an appropriate exercise prescription for each patient.
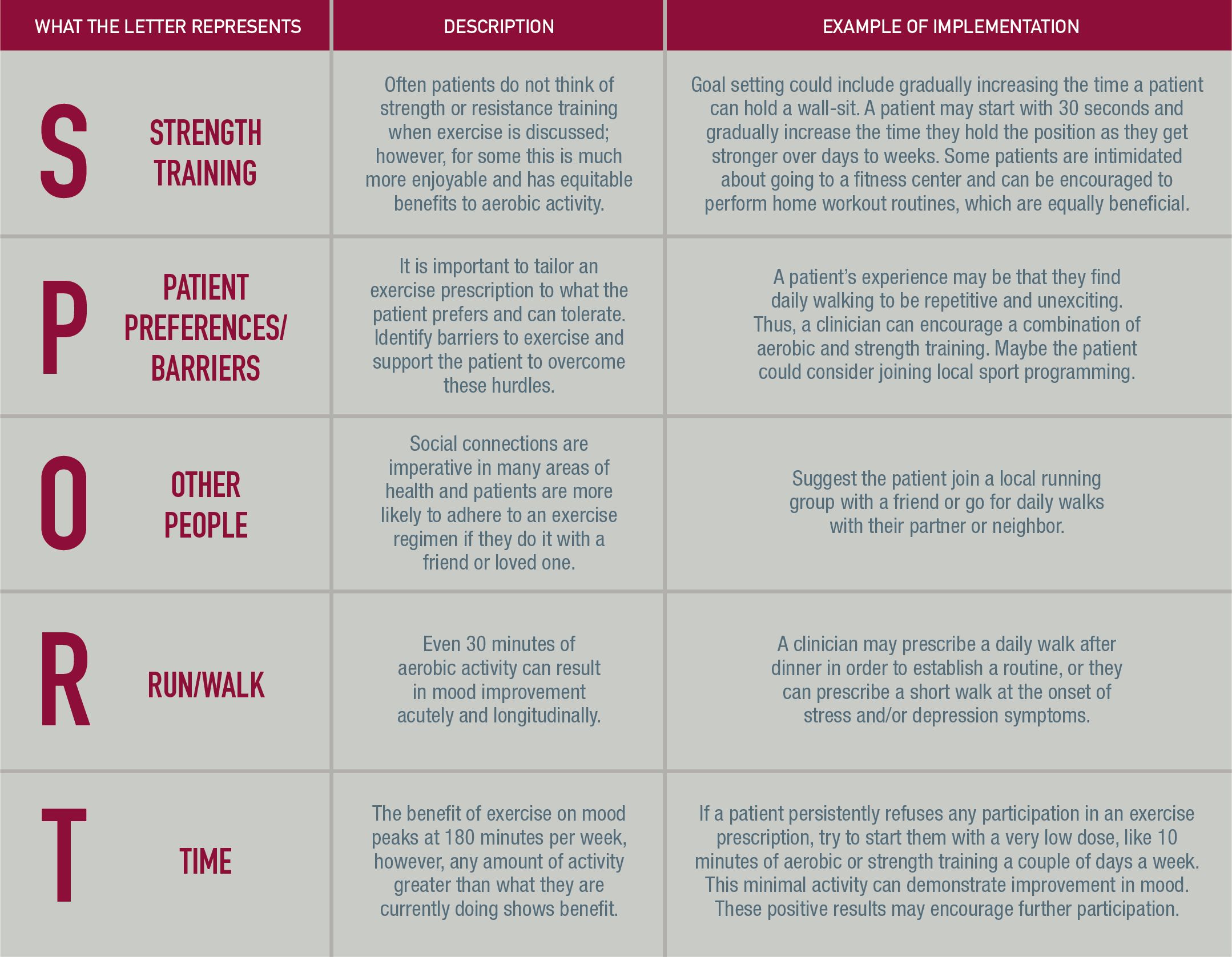
Table 2. The NICE Monoamine mnemonic demonstrates how a clinician can structure a discussion around the neurobiological implications of exercise and the mechanism behind the improvement of mood and cognition.
An exercise prescription is an important treatment option and a great adjunct to medications. The key is prescribing physical activity in a way that the patient will comply and remain engaged with. In psychiatry, we aim to improve our patient’s overall functioning biologically, psychologically, and socially. The various benefits of exercise extend well beyond improvement of mood. Applying the evidence and strategies discussed in this article will hopefully help reduce ambivalence in the patient and assist the busy clinician in implementing successful integration of exercise.
Mr Bergin is a medical student at the Michael G. DeGroote School of Medicine, McMaster University. Dr Noel Amaladoss is an assistant clinical professor at McMaster University and the Advanced Mind Clinic. Dr Antony Amaladoss is an assistant clinical professor at McMaster University and the Advanced Mind Clinic.
Do you incorporate exercise prescriptions in treatment strategies? Share you feedback: PTEditor@mmhgroup.com
References
1. Diaz K, Howard V, Hutto B, et al. Patterns of sedentary behavior and mortality in US middle-aged and older adults: A national cohort study. Ann Intern Med. 2017;167(7):465-475.
2. Chan J, Liu G, Liang D, et al. Special issue—Therapeutic benefits of physical activity for mood: A systematic review on the effects of exercise intensity, duration, and modality. J Psychol. 2019;153(1):102-125.
3. Harvey S, Overland S, Hatch S, et al. Exercise and the prevention of depression: Results of the HUNT cohort study. Am J Psychiatry. 2018;175(1):28-36.
4. Meyer J, Koltyn K, Stegner A, et al. Influence of exercise intensity for improving depressed mood in depression: A dose-response study. Behav Ther. 2016;47(4):527-537.
5. Dunn A, Trivedi M, Kampert J, et al. Exercise treatment for depression: Efficacy and dose response. Am J Prev Med. 2005;28(1):1-8.
6. Blumenthal J, Babyak M, Doraiswamy R, et al. Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosom Med. 2007;69(7):587-596.
7. Hoffman B, Babak M, Craighead W, et al. Exercise and pharmacotherapy in patients with major depression: One-year follow-up of the SMILE study. Psychosom Med. 2011;73(2):127-133.
8. Gordon B, McDowell C, Hallgren M, et al. Association of efficacy of resistance exercise training with depressive symptoms: Meta-analysis and meta-regression analysis of randomized clinical trials. JAMA Psychiatry. 2018;75(6):566-576.
9. Moraes H, Silveria H, Oliveria N, et al. Is strength training as effective as aerobic training for depression in older adults? A randomized controlled trial. Neuropsychobiology. 2020;79(2):141-149.
10. Oftedal S, Smith J, Vandelanotte C, et al. Resistance training in addition to aerobic activity is associated with lower likelihood of depression and comorbid depression and anxiety symptoms: A cross sectional analysis of Australian women. Prev Med. 2019;126:105773.
11. Singh N, Clements K, Fiatarone M. A randomized controlled trial
of progressive resistance training in depressed elders. J Gerontol A Biol Sci Med Sci. 1997;52(1):27-35.
12. Amiri S, Behnezhad S. Obesity and anxiety symptoms: A systematic review and meta-analysis. Neuropsychiatrie. 2019;33:72-89.
13. Knapen J, Vancampfort D, Morjien Y, et al. Exercise therapy improves both mental and physical health in patients with major depression. Disabil Rehabil. 2015;37(16):1490-1495.
14. Kanamori S, Takamiya T, Inoue S, et al. Exercising alone versus with others and associations with subjective health status in older Japanese: The JAGES Cohort Study. Sci Rep. 2016;6:39151.
15. Chaddock L, Erickson K, Prakash R, et al. A neuroimaging investigation of the association between aerobic fitness, hippocampal volume, and memory performance in pre-adolescent children. Brain Res. 2010;1358:172-183.
16. Hillman C, Buck S, Themanson J, et al. Aerobic fitness and cognitive development: Event-related brain potential and task performance indices of executive control in preadolescent children. Dev Psychol. 2009;45:114-129.
17. Seifert T, Brassard P, Wissenber M, et al. Endurance training enhances BDNF release from the human brain. Am J Physiol Regul Integr Comp Physiol. 2010;298:372-377.
18. Poulton N, Muir G. Treadmill training ameliorates dopamine loss but not behavioural deficits in hemi-parkinsonian rates. Esp Neurol. 2005;193:181-197.
19. Blomstrand E, Perret D, Parry-Billings M, Newsholme E. Effect of sustained exercise on plasma amino acid concentrations on 5-hydroxy-tryptamine metabolism in six different brain regions in the rat. Acta Physiol Scand. 1989;136:473-481.
20. Fordyce D, Farrar R. Enhancement of spatial learning in F344 rats by physical activity and related learning-associated alterations in hippocampal and cortical cholinergic functioning. Behav Brain Res. 1991;46:123-133.
21. Tsai C, Wang C, Pan C, Chen F. The effects of long-term resistance exercise on the relationship between neurocognitive performance and GH, IGF-1, and homocysteine levels in the elderly. Front Behav Neurosci. 2015;9:23.
22. Kleinloog J, Mensink R, Ivanov D, et al. Aerobic exercise training improves cerebral blood flow and executive function: A randomized, controlled cross-over trial in sedentary older men. Front Aging Neurosci. 2019;11:333.
23. Sparling P, Giuffrida A, Piomelli D, et al. Exercise activates the endocannabinoid system. Neuropsychol. 2003;17:2209-2211.
