- Vol 34 No 3
- Volume 34
- Issue 3
Your Money or Your Life: A Reflection on the Health Care Industry
Depression is the leading cause of disability worldwide, and this may indeed be the most telling legacy of the lost art of healing.
Francis Fukuyama1 famously declared that history ended on November 9, 1989. That was the date the Berlin Wall fell, the final victory of liberal democracy over every other form of government. The rest has been just a sorting through and biding time until all other governments come, in due course, to this realization.
According to Peter Sloterdijk,2 history ended on September 6, 1522. This was the day Ferdinand Magellan’s surviving crew, all 18 of them, sans Magellan, arrived back in Spain after circumnavigating the globe, thereby ushering in the era of “globalization” or the “post-history era.” Ever since, the rest has been a sorting out of the planet’s wealth by ruling oligarchies.
The nice thing about post-history is the opportunity it presents for a number of firsts. This is the first time there has been a broadly recognized health care crisis; this is the first time that health care has been referred to as an industry; in fact, this is the first time that medicine has been referred to as health care, with the implicit acknowledgment that medicine itself is a mere percentage of some greater enterprise. A medical megaplex-part physical structure, part ether-that by its very large-ness, its very enmeshment within an oligo-capitalist-informatic economy, has ceased to be an academic, philosophic, aesthetic, or noble endeavor.3 Insurers have ruled the day for less than a century, yet post-historically have come to dictate the practice of medicine: “Can you help me, Doc?” “Well, let me call your insurance company and see what we can do.”
So what is the role of the physician in this new post-historical age, this age of science, of neo-Enlightenment? Certainly in this age of cures, of solutions, the physician’s role is vastly different from that of his earlier counterparts. Before the age of cures-that is, when a physician was able to make and fulfill the odds-on promise of cure-he was bound to the patient’s bedside, as confessor and confidante, as a paternal figure of comfort and security. Indeed, the paternalistic model of the physician as authoritarian and dictator of patient care has long since fallen into disrepair-less through ineffectuality than semantic unkindness-in favor of a more insurance-friendly collaborative care model in which patient and physician agree upon a plan.
How might this work? The good post-historical doctor, with the advertising resources of the megalith at his or her disposal, above all must objectify the patient, must reduce him or her to an elemental story of biochemistry and pathology, must create only the slimmest measure of directed subjectivity within the patient. The real power of the post-historical physician is to grant the patient either a cherished or hated subjective experience.
Post-historical medicine of course is based on a legal-economic principle of autonomy, a principle without much historical basis, that views the individual as an isolated objective “unit” whose inner experience, once brought to said unit’s awareness, will allow the unit to make decisions in its own best self-interest. This model clearly only works in the context of a physician-patient relationship governed by the possibility of cure, where the physician actually holds something of value to the patient.
Still, there are many, if not a majority, of patients who wish nothing more than for their physicians to make medical decisions for them. Illness after all is a troubling subjective experience, mental illness near unbearable. It is little wonder the appeal of dissolution via narcotics or other drugs, meditation, death, or exotic religious experiences. Subjectivity is terrifying enough; more so in the face of disease. And subjectivity is certainly not to be equated with autonomy. One can act autonomously with little subjective experience. Similarly, one can maintain subjective experience in the midst of totalitarianism. The point here is that the subjectivity previously rendered by the physician now provides an illusion of autonomy against a perceived evil of paternalism.
The illusion of course is that of choice. Treatment options are presented with the full expectation that the patient will agree, similar to the illusion of choice in contractual agreements for other necessary services. In other words, a subjective experience common to all-if one needs such services, then one has no choice but to accept the proffered terms. Autonomy is after all a business concept, that aspect of an isolated objective unit that is targeted by media and is “open for business.” As a client is free to purchase the suggestions of a financial advisor, so a client purchases the suggestions of a physician. And given one’s inherent freedoms, one may well say “no thanks,” rendering the collaboration over-“see you later, no hard feelings.”
Patients did not generally free their physicians of moral obligations like this in the days before cures. Placebo after all relies on a paternal model. And although a patient with his wits about him was perfectly aware he was nothing more than an object to his physician, he needed this objectification in order to verify his experience, to maintain the awareness of his unconscious, to prepare himself either to pass on, or to generate the resources to recover. Compassion was meted out judiciously, and a good physician was more expert in the course of disease, and the expected signs and symptoms. The role of the hospital was minimal, and the emergency department didn’t exist until well into the 20th century.
In the age of cures, the physician is responsible for creating and maintaining an experience of “illness” among patients. This is reinforced by the pharmaceutical industry that relies on patients wanting drugs. And all is overseen and regulated by the institutional cruelty of the insurance industry: “Did the patient actually have a gun in his mouth?” “Yes.” “Was it loaded?” “I’m not sure.” “Then the best we can do is authorize one day in the hospital.”
Only the psychiatrist with his empty doctor’s bag and his lack of treatment algorithms has the ability to stand outside this system, to throw a wrench into the capital-dependent health care machinery. The non-psychiatric physician wants no part of de-constructing the subjective reality of the patient. The fantasy of illness keeps the machine moving. The psychiatrist on the other hand is charged with challenging the very subjective fantasies of the patient, with uncovering the non-fantastic inner experience that may in fact be closer to the truth of that patient.
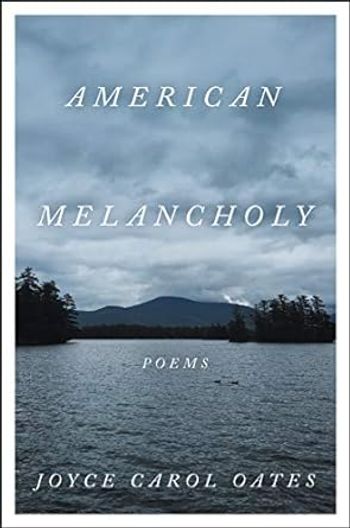
Typically what is uncovered is depression, more colorfully described by some as “strange sadness” or “fundamental melancholy.”4 In other words, mortality. In an age where self-absorption is advertised, encouraged, lauded, and at times fantastically rewarded-in an operant conditioning sort of way-the fact that such is a cardinal symptom of depression proper is passed over as non-expedient. This is not to say that depression as an illness is not easily treated pharmacologically, but the fundamental nature of this depression, this melancholy, this hopelessness is not-and cannot be-addressed by a health care machine.
The thoughtful psychiatrist then finds himself living in “history,” more akin to the paternalistic physician, the priest, the witch, the alchemist of yore. Indeed the psychiatrist remains on the fringes of the current medical model, not so much accommodated as tolerated by the health care machinery, allowed to prescribe, but contained to 15 minutes. Like limiting the confessional to 15 minutes, and these are constraints utterly beyond the foresight of earlier philosopher-physicians. How is the future supposed to interpret this? And worse, how will the future interpret the agreed-upon solution? With denial; complete, utter denial.
Cognitive behavioral therapy is covered by insurance precisely because denial is this treatment’s stated goal. That is, it facilitates patients’ denial of their own subjective experience. Good old-fashioned psychoanalysis, on the other hand, is designed to uncover one’s subjectivity from amid the ruins of an unconscious truth. A more complicated process, not easily explained to third-party payers and with less easily shown outcomes, psychoanalysis is not covered. The treatment, as envisioned by Freud in a pre-third party payer era, took root at the end of an epoch that provided a broad, humanistic education to its physicians. This also coincides with Darwin’s destruction of the remnants of Christianity via the dissemination of evolutionist principles. Evolution effectively demolished the preconceived longings, hopes, and prophecies of the past. Faith as a measure unto itself was rendered insignificant, and science took over.
So how will trust-fund scholar-futureniks interpret the health care megalith that was once a simple physician-philosopher construct? Post-historical medicine is an industry, an inquisitorial bureaucracy, legislated by treatment algorithms and standards of care easily interpreted by physicians, patients, insurers, and judges. There is no magic; even placebo has been quantified.5 Insurers, whose decision-makers remain remote and anonymous, dictate the practice of medicine from on high. The government has put a price on human life, and the vast majority of a physician’s day is spent documenting evidence.6 Efficiency is rewarded, and time itself has become the most highly prized commodity.
Memorization is easy, and algorithms make medicine very easy. Advertising makes medicine even easier; and the Internet makes medicine downright facile: “What do you think is wrong with you?” “I looked it up online, and I think I have such and such.” “Okay, I can prescribe you this or that.” “Actually I saw this advertised on television, and I would like to try it.” “No problem. We can do that.” The capability of performing Google searches is misinterpreted as the action of an educated consumer, of a “citizen-scientist.”7
Luckily for both patients and physicians, the one thing that has not changed over the centuries is the remarkable ability of the human body to heal itself.8 Unfortunately for both patients and physicians, however, the fractured mind remains mostly resistant to cure. Imagine conquering death, only to live with unrelenting anguish. Depression is the leading cause of disability worldwide, and this may indeed be the most telling legacy of the lost art of healing.9 Perhaps it is true that the more things change, the more they remain the same.
MORE ABOUT Elliott B. Martin Jr, MD
If indeed Ambrose Bierce is correct that learning is the kind of ignorance that distinguishes the studious, then let me offer myself as example.
As a younger man, I remember opening Doctor Louis-Ferdinand Auguste Destouches’s pseudo-autobiographical novel, Journey to the End of the Night-sometimes the sequel, sometimes the prequel to Death on the Installment Plan-at a time when I was so down and out as to have started ruminating over military heroics. Dr. Destouches of course is better known by his celebrated pseudonym, Céline. (A modest gentleman, he famously declared Jean Genet the second greatest writer in France.)
This was even before my other, brief life in academia, a time when I lived nobly, purely, as a struggling writer. Like the author, I was over-educated and under-employed. I ate sparingly, and had somehow procured a degree in science along the way. Of all things, the thought of medical school had also intruded here and there.
But I resisted. Like Louis-Ferdinand, I wished to be destined for bigger things. If not to be a great writer, then at least a great pamphleteer, inciter, rabble-rouser, arm in arm with Doctor Thomas Young and Thomas Paine.
And so it was that I fidgeted youthfully, embarrassingly really, for my age, and read random lines, first of the author’s watching the bandwagon roll by and contemplating whether it would be worth his while to enlist in the French army at the start of World War I. Inspired, I remember thinking, this guy really became a doctor?
I skipped and flipped madly, merrily, back and forth, savoring the halting, redundant prose. Here was someone else, a dreamer trapped among the bizarre choices of medical school versus the military versus a random life . . . .
And the rest is post-history.
Disclosures:
Dr. Martin reports no conflicts of interest concerning the subject matter of this article.
References:
1. Fukuyama F. The End of History and the Last Man. New York: Free Press; 1992.
2. Sloterdijk P. In the World Interior of Capital: For a Philosophical Theory of Globalization. Cambridge, UK: Polity Press; 2013.
3. Cohn J. Sick: The Untold Story of America’s Health Care Crisis and the People Who Pay the Price. New York: Harper Perennial; 2008.
4. Žižek S. The Fragile Absolute: or Why Is the Christian Legacy Worth Fighting For? London, New York: Verso; 2008:80-83.
5. Hróbjartsson A, Gøtzsche PC. Is the placebo powerless? An analysis of clinical trials comparing placebo with no treatment. N Engl J Med. 2001; 344:1594-1602.
6. Regulation: putting a price on life. The Week. February 23, 2011.
7. Gorey C. 5 Apps to Help You Become a Citizen Scientist With Nearly Minimal Effort. October 24, 2016.
8. Goldstein K. The Organism: A Holistic Approach to Biology Derived From Pathological Data in Man. New York: Zone Books; 1995.
9. Ferrari AJ, Charlson FJ, Norman RE, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med. 2013;10:e1001547.
Articles in this issue
almost 9 years ago
Psychogenic Non-Epileptic Seizures: Clinical Issues for Psychiatristsalmost 9 years ago
Update on Medical Catatonia: Highlight on Deliriumalmost 9 years ago
Depression and Anxiety Disorders in Patients With Canceralmost 9 years ago
THE QUIZ: Headachesalmost 9 years ago
Westworld: Hell Hath No Limitsalmost 9 years ago
Sound of Silencealmost 9 years ago
Maintenance of CertificationNewsletter
Receive trusted psychiatric news, expert analysis, and clinical insights — subscribe today to support your practice and your patients.