
The potential of TMS as a treatment for cognitive disorders, fatigue, pain, and other manifestations of brain disease is discussed, as is the encouraging prospect for neuropsychiatric management of many patients.


The potential of TMS as a treatment for cognitive disorders, fatigue, pain, and other manifestations of brain disease is discussed, as is the encouraging prospect for neuropsychiatric management of many patients.

This case stresses the importance of identifying cultural issues that arise in mental health clinical encounters.

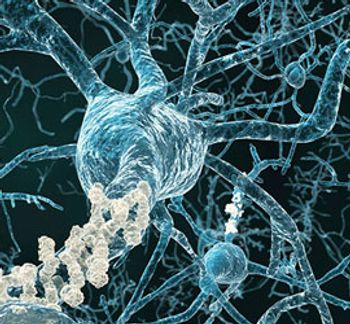
The SSRIs, although principally targeting serotonin transporter, are complex drugs that might work on other neurotransmitter and receptor systems. It is likely worthwhile to look at the effects of other monoamine and neuropeptide systems on the enzymatic machinery cleaving the amyloid precursor protein.

Vascular surgeons, internists, and neurologists all exist-but why aren’t there any vascular psychiatrists? There certainly is a need.

In the trenches of Alzheimer research, the battle continues . . . but where do we stand? Is the war on AD dementia nearing conclusion, or are we simply in the initial throes of the fight? Three experts weigh in.
Alzheimer disease psychosis appears to be a distinct clinical entity. This article focuses on management strategies.

Demographic shifts and rising life expectancies will lead to an epidemic of chronic neuropsychiatric disease, and societal and public health costs will be enormous. Deep brain stimulation--a procedure that interfaces directly with the neural elements that drive pathological behavior--could be useful.

Big things are happening in Alzheimer disease research. Recent developments are shaping the future for assessment and diagnosis and allowing for early detection and treatment of the disease.

While the growing evidence base for the positive effects of lithium on brain health is compelling, the evidence remains preliminary.

We have the target protein for Alzheimer, the antibody to knock out the protein, and the imaging test locating the protein in the brain, but there still remains one problem . . . who should receive the antibody?

Results of a 10-week prospective study, recently reported at the Annual Meeting of the American Association for Geriatric Psychiatry, offered no conclusive evidence about the mortality risk of elderly patients with Alzheimer disease who were treated with antipsychotics.

Despite the prevalent perception that cognitive decline in the aged population is inevitable, researchers with Northwestern University's SuperAging Project are finding that "excellent memory capacity in late life is a biological possibility."

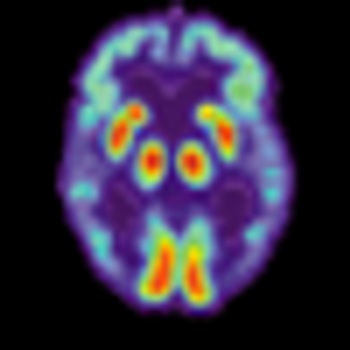
Because of new imaging techniques and advances in our understanding of neurophysiology, neurological and psychiatric disorders are increasingly being recognized as disorders of circuit functions in the brain. Using techniques such as DBS, neurosurgeons are able to pinpoint malfunctioning circuits and to recalibrate them.

Less common but still important syndromes connected with Alzheimer disease include traumatic brain injury, infectious and inflammatory disorders, alcohol-induced dementia.
The evolution of deep brain stimulation for various neuropsychiatric disorders results from advances in structural and functional brain imaging, increased understanding of neurocircuitry of the brain, and improvements in neurosurgical techniques and equipment.

The proposed new diagnostic categories and guidelines for Alzheimer's disease include not only dementia, but also the preclinical and mild cognitive impairment (MCI) phases of AD.

Medical professionals may be reluctant to initiate a discussion about driving with older patients in anticipation of a negative impact on the physician-patient relationship.

New diagnostic guidelines and advanced screening tools enable clinicians to detect dementia and Alzheimer disease earlier than ever.

Age is a major risk factor for the development of Alzheimer disease and other dementias. New technologies in brain imaging represent major advances in our ability to diagnose age-related cognitive and behavioral disorders.

While there are currently no treatments for AD, it is important to examine what we are treating. By the time AD is diagnosed by clinical symptoms, 8 to possibly 15 years of pathological damage has already occurred.

Anton Porsteinsson, MD, discusses some specifics for fine-tuning the care of patients with Alzheimer disease. Here: optimizing physical health and mental stimulation and promoting a brain-healthy diet and aerobic exercise.

Can stimulants increase function in people with early stage Alzheimer disease? Here, Anton Porsteinsson, MD, discusses the pros and cons.

In this video, Anton Porsteinsson, MD, discusses some of the causative factors of Alzheimer disease: genetics, environment, personality. He goes on to explain that although there are clear determinants for AD, there are preventive actions that can be taken to delay the onset of disability.

The Alzheimer’s Association announced in July that the FDA had accepted its recommendations to modify exclusion and monitoring criteria for clinical trials of agents that affect β-amyloid protein in the brain.
If telling patients they have “pre-clinical Alzheimer’s” or “MCI due to Alzheimer’s Disease”-absent effective treatment-produces more emotional suffering than it relieves, a difficult ethical question arises; namely, can such a disclosure be justified under the foundational principle of non-malfeasance?