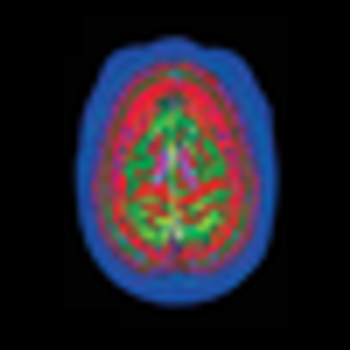
The causes of Alzheimer disease and attempts to predict who is at risk for it have been confounding the medical profession ever since Dr Alzheimer first described the disorder in 1906. Finally, a breakthrough in dye and imaging technology may be the key to solving the puzzle.






