
Sleep Deprivation
Latest News
Latest Videos
CME Content
More News

From herbal medicine for psychiatrists to the psychiatric implications of the Parkland School massing shooting, here are highlights from the week in Psychiatric Times.

How can knowledge—and positive attitudes—about sleep improve quality of life for patients?

Sleep problems are understudied, underdiagnosed, and undertreated.

This investigational dual orexin receptor antagonist improved sleep overnight and daytime functioning.

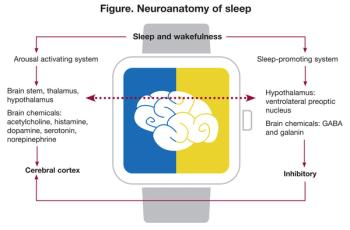
The associations between sleep/rhythms and psychiatric disorders are not well understood. With additional research we can better address key issues and improve patient outcomes.

The steadily rising rate of suicide in the US is a vexing public health crisis. Among the many risk factors for suicidal thoughts and behaviors is sleep disturbance.

Here's a brief history of sleepwalking, associated factors, and pathology; sleep-related violence and forensic considerations; and management strategies.
Here's an update on parasomnias-the undesirable physical, experiential, or behavioral phenomena that occur exclusively during sleep onset, during sleep, or during arousals from sleep.

All psychiatrists know the risk factors for suicide. Among the newest modifiable risk factors to join the list are insomnia and nightmares.

Sleep disorders represent a significant problem in patients with Alzheimer disease. Here: assessment strategies and a review of drug and non-drug interventions.
Sleep-related problems are among the most disabling consequences of TBI, with multiple influences: impairment of neuronal plasticity, metabolomic alterations, loss of vascular homeostasis, and disruption of the blood-brain barrier. The authors take a close look.

What's new in sleep medicine? The latest developments in both new and novel approaches to treating sleep disorders.

Astrocytic signaling to adenosine receptors results in the robust reduction of depressive-like behaviors associated with sleep deprivation.

Insomnia-a sleep disorder that can pose impairments far more debilitating than than problems with cognition (eg, difficulty processing, unclear thinking).

Sleep-disordered breathing is common in patients with mood and anxiety disorders. This article explores the implication for practicing psychiatrists whose patients have sleep disorders.

Sleep changes associated with psychotropic drugs are common enough to justify routinely obtaining a baseline sleep diary before beginning treatment, even when the initial screening for sleep disorders indicates that no further investigation is needed.

Can you name an important part of good sleep hygiene? The use of which short-acting sedative-hypnotics to treat sleep disturbances in patients is associated with Alzheimer disease? These questions and more.

The plain fact is that nothing that has been claimed in the name of defending our country can justify cruel, inhuman, and degrading treatment of another man or woman. Torture, in any form-light or heavy-is not a tool of interrogation or useful for gathering good intelligence.

Keys to diagnosis, assessment, and management.

During my medical training in the early 1980s, I attended a Grand Rounds on health care reform. Sleep-deprived physicians-in-training are easily conditioned to snooze upright in their auditorium seats, and economics is not an interest of choice for me, but when the speaker told us that there would be no solution to rising health care costs except to fracture the bond between patient and doctor, I found myself engaging in nightmarish fantasies that in subsequent decades have come true.

On Monday, August 24, 2009, in response to a Freedom of Information Act lawsuit, the Central Intelligence Agency (CIA) released a “Top Secret,” highly redacted May 7, 2004, report, Counterterrorism Detention and Interrogation Activities (September 2001 – October 2003).1 The report’s opening pages concede that the activity it divulges “diverges sharply from previous Agency policy and rules that govern interrogation.”

Surveys show that approximately 60% of the general population has gambled within the past 12 months.1 The majority of people who gamble do so socially and do not incur lasting adverse consequences or harm. Beyond this, approximately 1% to 2% of the population currently meets criteria for pathological gambling.2 This prevalence is similar to that of schizophrenia and bipolar disorder, yet pathological gambling often goes unrecognized by most health care providers.

As we begin this brief review of the neurobiology of major depressive disorder (MDD), we face these fundamental questions

Because numerous diseases- infectious, endocrinological, metabolic, and neurological, as well as connective-tissue disease-can induce psychiatric and/or behavioral symptoms, clinicians need to distinguish these neuropsychiatric masquerades from primary psychiatric disorders, warned José Maldonado, MD, the director of Stanford University’s Psychosomatic Medicine Service.

I am writing to correct several inaccurate assertions in the essay, “The American Psychological Association and Detainee Interrogations: Unanswered Questions” (Psychiatric Times, July 2008, page 16), by Kenneth S. Pope, PhD, and Thomas G. Gutheil, MD.










