The articles in this Special Report provide a broad, cross-cutting perspective on the current state of addiction psychiatry, insofar as it may pertain to your own clinical practice.
The articles in this Special Report provide a broad, cross-cutting perspective on the current state of addiction psychiatry, insofar as it may pertain to your own clinical practice.

The loss of control over urges and behaviors may be the central component of gambling disorders, but there is so much more to consider. Individuals with these problems have exponentially higher rates of suicide attempts and completions.

Many people like to spend at least part of their free time playing video games. However, for some, what starts as innocent recreation becomes an addiction and, at times, tragedy ensues.

Pathological gambling is a common psychiatric condition that can present with a variety of symptoms. Treatment recommendations available for pathological gamblers, as well as resources for patients and their families in this Tipsheet.

Impulse control disorders are common psychiatric conditions in which affected individuals typically report significant impairment in social and occupational functioning, and may incur legal and financial difficulties as well.

Are there differences in the neuroimaging of persons who just gamble and those who pathologically gamble?

A panel of experts at the APA Annual Meeting discussed how changes in DSM-5 may affect clinical practice. Highlights here.

"Internet Addiction" may soon spread like wildfire. All the elements favoring fad generation are in place . . . the profusion of alarming books; the breathless articles in magazines and newspapers; extensive TV exposure; ubiquitous blogs; the springing up of unproven treatment programs; the availability of millions of potential patients; and an exuberant trumpeting by newly minted "thought leading" researchers and clinicians. So far, DSM-5 has provided the only restraint.

Data from neurobehavioral studies, brain imaging studies, epidemiological surveys, and clinical trials show that pathological gambling shares aspects of both impulsivity and compulsivity.

A video on ADHD and impulsivity from childhood to adulthood.

The paradigm for modern psychiatry is evidence-based medicine (EBM)-it represents proven treatments for defined diagnoses. But there are major problems with this position, starting with the fact that while they are superior to placebo, evidence-based treatments too often are ineffective.

Advances in the fields of neuropsychological assessment and neuroimaging have enormously expanded our knowledge about the profile and severity of cognitive deficits in patients with substance use disorders.

I would like to start off this blog with two stories that happened many years ago.

Although Charles O’Brien, MD, who heads the substance-related disorders work group, is a vigorous proponent of the notion of addiction as a disease, nothing about the proposed DSM-5 substance-related disorders section supports the idea that the syndrome is best understood as a chronic brain disease.
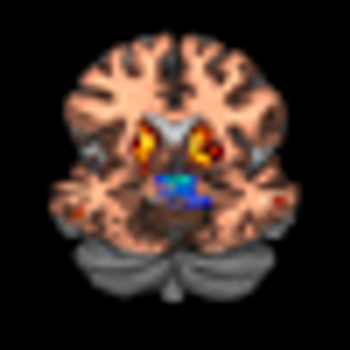
A brief report recently published in Science confirms the key role of dopamine (DA) in impulsive behavior. The researchers found that impulse control directly correlated with the amount of DA released in the striatum.

The recently posted first draft of DSM-5 has suggested a whole new category of mental disorders called the "Behavioral Addictions." The category would begin life in DSM-5 nested alongside the substance addictions and it would start with just one disorder (gambling).

Parkinson disease (PD) is the second most common neurodegenerative illness in the United States, affecting more than 1 million persons. Disease onset is usually after age 50. In persons older than 70 years, the prevalence is 1.5% to 2.5%.1 While the primary pathology involves degeneration of dopaminergic neurons in the substantia nigra, circuits important in emotion and cognition-such as the serotonergic, adrenergic, cholinergic, and frontal dopaminergic pathways-are also variably disrupted.

To Americans over 30, YouTube, Facebook, MySpace and Twitter are buzzwords that lack much meaning. But to those born between 1982 and 2001-often referred to as “millennials” or “Generation Y”-they are a part of everyday life. For the uninitiated, these Web sites are used for social networking and communication. They are also places where individuals can post pictures and news about themselves and express their opinions on everything from music to movies to politics. Some sites, such as YouTube, allow individuals to post videos of themselves, often creating enough “buzz” to drive hundreds and even thousands of viewers; in some instances, these videos create instant media stars-such as the Obama imitator, Iman Crosson.

Self-administration of drugs of abuse often causes changes in the brain that potentiate the development or intensification of addiction. However, an addictive disorder does not develop in every person who uses alcohol or abuses an illicit drug. Whether exposure to a substance of abuse leads to addiction depends on the antecedent properties of the brain.

Surveys show that approximately 60% of the general population has gambled within the past 12 months.1 The majority of people who gamble do so socially and do not incur lasting adverse consequences or harm. Beyond this, approximately 1% to 2% of the population currently meets criteria for pathological gambling.2 This prevalence is similar to that of schizophrenia and bipolar disorder, yet pathological gambling often goes unrecognized by most health care providers.

Fewer than a handful of books have been published on the ethical dimensions and challenges in treating and helping persons living with an addiction. Therefore, this book is a welcome contribution to the literature almost from the start. The contributors in this 9-chapter text range from community- and hospital-based professionals to behavioral program directors to ethics center directors and researchers to psychology, neurology, and psychiatry professors and fellows. The book aims to provide general advice on central issues encountered routinely by those experienced in addiction services and research. Contrary to the book’s rather biblical and authoritative title, the editors “offer this work modestly,” given the relative newness of focused ethical analysis in addiction treatment and care.

DSM-IV-TR, our current diagnostic classification system of psychiatric disorders, follows the diagnostic paradigm first established by DSM-III in 1980.

Recent research has raised concerns about the adequacy of psychiatric diagnostic evaluations conducted in routine clinical practice, particularly the detection of disorders that are comorbid to the principal diagnosis.

Diagnostic assessment of psychiatric disorders and their comorbidities is a challenge for many clinicians. In emergency settings, there is no time to conduct lengthy interviews, and collateralinformation is often unavailable.

Emergency medicine provides care to a vast number of patients each year. In 2005, 115.3 million people visited emergency departments (EDs).