Publication
Article
Psychiatric Times
Convergence Mental Health: A New Pathway for Transdisciplinary Innovation and Entrepreneurship
Author(s):
A paradigm shift is needed in order to solve the unprecedented complexities and challenges associated with the current global mental health crisis.
envfx/AdobeStock

PSYCHIATRY 20/20
Modern mental health problems are characterized by their complexity, multi-systemic nature, and broad societal impact, hence making them poorly suited to siloed approaches of thinking and innovation. The New England Journal of Medicine recently published an article that articulated the stark limitations of an increasingly siloed focus on biologic knowledge in psychiatry.1 The article describes how the biological revolution of the 1980s has failed to live up to its therapeutic or scientific promise, with a comprehensive biologic understanding of the causes or treatments of psychiatric disorders yet to be discovered. Further, the article argues that psychiatry faces a new set of challenges, such as a professional diagnosis being reduced to a “checklist-style amalgamations of symptoms,” and an alarming degree of “trial-and-error medication management” taking over practice.
Psychiatry is characterized by multiple complex interacting, biological, social, medical, psychological, and related systems. Consequently, it is important to note that these challenges are not nostalgic arguments for a return to the insular, often unscientific psychodynamic practice of psychiatry that marked the 20th century. Instead, they indicate the need to forge a new path, one with an approach ready to meet the unprecedented and complex systemic mental health challenges of the 21st century.
Indeed, the 21st century will be largely defined by our collective response to the global mental health crisis. According to a recent World Health Organization (WHO) report, around 450 million people currently suffer from mental health conditions, making brain disorders among the leading causes of ill health and disability worldwide. The world’s failure to respond to the mental health crisis has resulted in a “monumental loss of human capabilities and avoidable suffering.”2 Many of these issues will be magnified by COVID-19 that will result in social and physical distancing, economic hardship, and challenges in accessing care (Table 1).
A paradigm shift is needed in order to solve the unprecedented complexities and challenges associated with the current global mental health crisis. Indeed, scientific progress may be seen as “a series of peaceful interludes punctuated by intellectually violent revolutions.”3 A convergence science approach is needed to address the global mental health crisis, bringing about an urgently needed revolution in science and society.
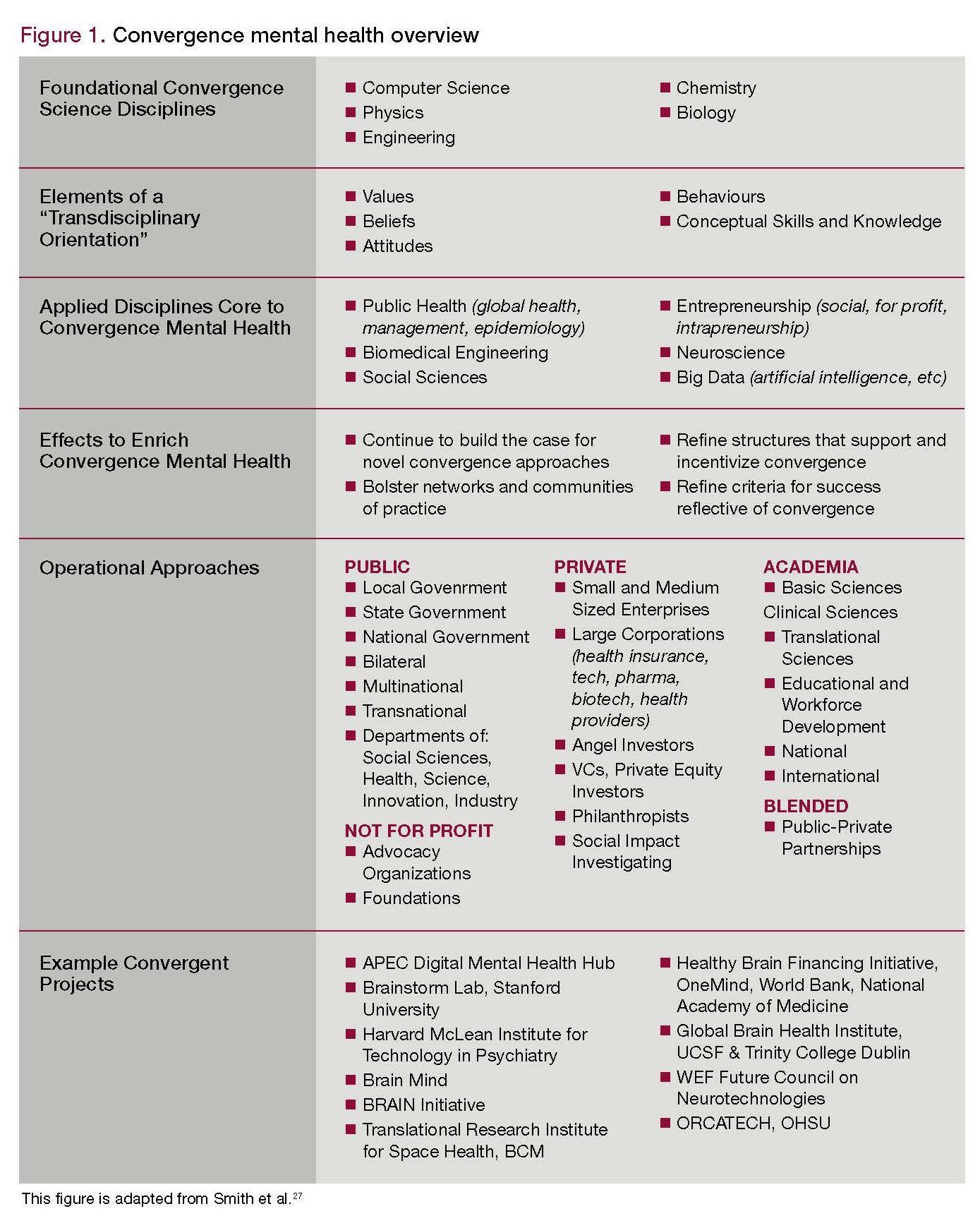
Convergence science integrates knowledge, tools, and thought strategies from various fields for tackling challenges that exist at the interfaces of multiple fields.4 In the context of mental health, convergence involves the integration of scientists, clinicians, bioinformaticists, global health experts, engineers, technology entrepreneurs, medical educators, caregivers, and patients. Synergy between government, academia, and industry is also vital. Convergence mental health is the approach used for mental health (Table 2).
Innovation and entrepreneurship with convergence science
COVID-19 can provide a framework for a convergence science approach to tackling the global mental health crisis. Akin to COVID-19 efforts, solutions to the global mental health crisis will require the traditional sciences of chemistry, biology and virology, and the new sciences of big data and artificial intelligence, computer science and statistical models, and -omics medicine. Subsequently, solutions will need sociologists, psychologists, philosophers, ethicists, scientists, media practitioners, crisis management experts, policy makers, and senior civil servants.
The demands of today’s global problems—especially the mental health crisis—also necessitate a fundamental shift in approaching education and workforce development. Individuals in a convergence science workforce must be equipped with deep expertise in their field, while also having literacy and understanding across a broad range of disciplines necessary for transdisciplinary collaborations.5,6
We must be willing to rethink education and training for researchers, clinicians, and others within traditional health care fields. Education needs to shift toward skill sets adaptable to diverse problems. Unconventional skills and topics, such as design thinking, entrepreneurship, computer science, cryptography, and the like, could be incorporated into learning. Creative education opportunities such as mini-fellowships or exchanges may facilitate divergent thinking.
Traditional education pathways as the sole means of involvement in mental health research must also be reconsidered. To develop innovative solutions, a diverse array of solvers is needed. Collective intelligence—including citizen scientists—must be leveraged. Bansho, the Japanese method of collective problem-solving, teaches people to grasp connections and progressions of the thinking needed to develop solutions. It may provide a framework for education and training modules for convergence science researchers.
In 2001, InnoCentive was co-founded by Alph Bingham, PhD, and Aaron Schacht to crowdsource solutions to the most intractable solutions.7 As a space for dialogue between specialists and industry outsiders was created, fresh ideas to persistent questions were found. A chemist from Illinois, John Davies, was able to use an idea from his earlier career in construction to help solve the cleanup of the Exxon Valdez oil spill on Alaska’s coast.8 Other organizations have also utilized the InnoCentive model, including Kaggle, which is dedicated to problems in machine learning.9 Both InnoCentive and Kaggle have methods that are currently being adapted to develop solutions for COVID-19 related issues and could be used to develop mental health solutions in the future.
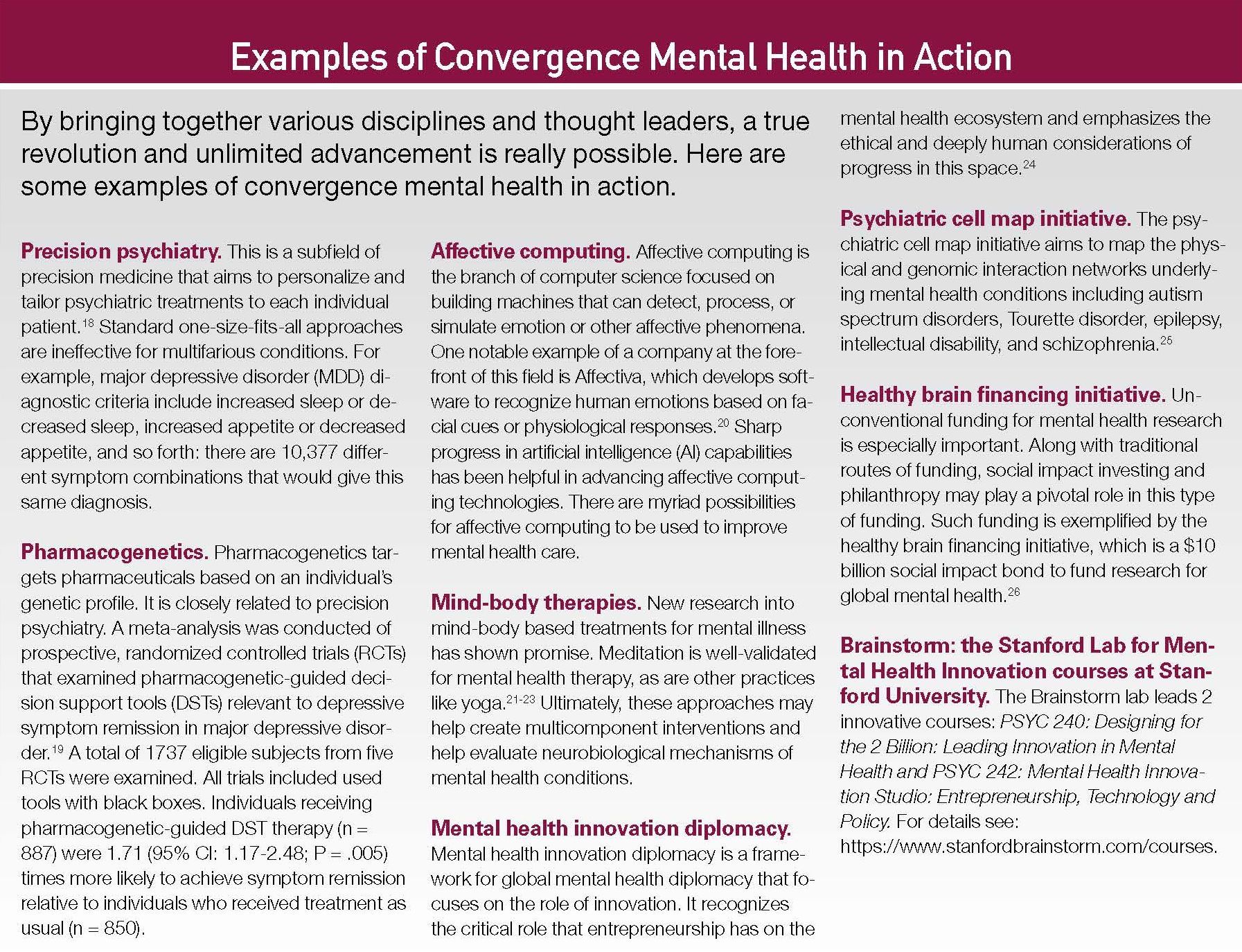
In low- and middle-income settings, where there are few psychiatrists, greater deployment of community health workers is important to provide essential care. This requires transdisciplinary thinking. A recent clinical trial explored the role of lay counsellors in providing a “depression in later life” intervention in Goa, India.10 In this randomized clinical trial, lay counselors provided problem-solving therapy, brief behavioral treatment for insomnia, education in self-care of common medical disorders such as diabetes, and assistance in accessing medical and social programs. The intervention was effective for preventing episodes of major depression in older persons with subsyndromal symptoms. Furthering the reach of lay counsellors, promising trial data now show the value of internet- based behavioral activation with lay counsellor support for the treatment of depression.11
A convergence workforce adept at navigating the adoption of new technological innovations is especially important. Technology will continue to fundamentally shift the way we conceptualize and treat mental health conditions. For example, Mindstrong aims to provide continuous digital biomarkers of mood and cognition to support diagnosis, prognosis, and treatment monitoring.12 Born from convergence science, Mindstrong originated from prior work of co-founder Paul Dagum, MD, PhD, in cybersecurity. Adopted for mental health conditions, it may make it possible to detect prodromal stages of mental health conditions, enabling objective measurements and the opportunity for early intervention and prevention.
The same technologies used for early detection and monitoring may also be used to deliver treatment and interventions. For example, Akili Interactive Labs builds clinically validated cognitive therapeutics, assessments, and diagnostics that look and feel like video games and has submitted prescription video games for people with attention-deficit/hyperactivity disorder for FDA approval.13,14 A recent review of the mental health technology field projected there will be 1000 mental health startups by the end of 2020.15 See the Examples of Convergence Mental Health in Action at the end of this article for more information.
Conclusion
The progress in technological advancements like the printing press and developments in science, art, philosophy, and trade that underpinned the Renaissance period was sparked by a convergence approach that merged science and humanities.16 A similar revolution will occur with convergence mental health solutions, ensuring greater integration of social sciences in care. Mental health is an inherently human undertaking. Indeed, convergence mental health should employ considerations from the new field of responsible innovation in mental health, which is “a collaborative endeavor wherein stakeholders commit to clarifying and meeting a set of ethical and social principles by designing solutions to sustainably address the needs and challenges of mental health systems.”17
Convergence mental health must also address the social determinants of health and be mindful of the world’s immense cultural diversity. Addressing the social determinants and cultural components of mental health requires rethinking our concept of disease and integration among health systems, local community partners, and coordination at a national or international level. Ensuring that there is a place for social science is critical to achieve a convergence approach and provides an opportunity to prevent mental health disorders, improve mental health at a population level, and reduce social and health inequalities.
Psychiatry has a major opportunity to leverage convergence science that will lead to innovation and progress. Ultimately, convergence mental health will help usher in a new era of care marked by bridging the divergent fields of medical practice, integrating insights from the brain and mind. Convergence mental health holds the potential to integrate technological innovations, insights from other areas of medicine, paradigmatic research shifts that blur existing boundaries between academia and industry, social determinants of health, philanthropy, and unconventional funding mechanisms. These changes will result in better patient outcomes and ensure greater health justice for all people by preparing psychiatry to meet the unprecedented mental health challenges of the 21st century.
Examples of Convergence Mental Health in Action
We hope to offer brainstorming opportunities and solutions in our forthcoming book, Convergence Mental Health: A Roadmap Towards Transdisciplinary Innovation and Entrepreneurship, scheduled for publication in late 2020. We only hope to keep up with the world that is rapidly changing in front of our eyes.
Ms Smith is Brain Health Venture Executive, Founder and CEO, FacePrint, and Mr Ellsworth is Affiliate, Department of Computer Engineering Stanford University, Palo Alto, CA. Dr Reynolds is Distinguished and Emeritus Professor of Psychiatry, University of Pittsburgh, Pittsburgh, PA. Dr Berk is Professor of Psychiatry, Deakin University, IMPACT, The Institute for Mental and Physical Health and Clinical Translation, School of Medicine, Barwon Health, Geelong, Australia; Department of Psychiatry, ORYGEN Youth Health, The Florey Institute for Neuroscience and Mental Health, University of Melbourne, Victoria, Australia. Dr Eyre is Instructor in Entrepreneurship, Global Brain Health Institute (UCSF and Trinity College Dublin); Deakin University, IMPACT, The Institute for Mental and Physical Health and Clinical Translation, School of Medicine, Barwon Health, Geelong, Australia; Department of Psychiatry, University of Melbourne; Brainstorm Laboratory for Mental Health Innovation, Department of Psychiatry, Stanford University School of Medicine, Palo Alto, CA; and Discipline of Psychiatry, School of Medicine, The University of Adelaide, Adelaide, South Australia, Australia. Dr Lavretsky is Professor of Psychiatry, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles, CA. The authors report no conflicts of interest concerning the subject matter of this article.
Acknowledgements—Dr Berk is supported by a NHMRC Senior Principal Research Fellowship (1059660 and 1156072).
References
1. Gardner C, Kleinman A. Medicine and the mind: the consequences of psychiatry’s identity crisis. New Eng J Med. 2019;381:1697-1699.
2. Patel V, Saxena S, Lund C, et al. The Lancet Commission on global mental health and sustainable development. Lancet. 2018;392:1553-1598.
3. Kuhn TS. The Structure of Scientific Revolutions. Chicago and London: Chicago University Press; 1962.
4. Council NR. Convergence: Facilitating Transdisciplinary Integration of Life Sciences, Physical Sciences, Engineering, and Beyond. Washington, DC: National Academies Press; 2014.
5. Page SE. The Model Thinker: What You Need to Know to Make Data Work for You. Hachette UK: Basic Books; 2018.
6. Parrish S, Beaubien R. The Great Mental Models: General Thinking Concepts. Minneapolis, MN: Latticework Publishing Inc; 2019.
7. InnoCentive. https://www.innocentive.com.
8. Epstein D. Range: Why Generalists Triumph in a Specialized World. Riverhead Books. 2019.
9. Kaggle. https://www.kaggle.com.
10. Dia A, Azariah F, Anderson SJ, et al. Effect of a lay counselor intervention on prevention of major depression in older adults living in low- and middle-income countries: a randomized clinical trial. JAMA Psychiatry. 2019;76:13-20.
11. Arjadi R, Nauta MH, Scholte, WF, et al. Internet-based behavioural activation with lay counsellor support versus online minimal psychoeducation without support for treatment of depression: a randomised controlled trial in Indonesia. Lancet Psychiatry. 2018;5:707-716.
12. Carey B. California tests a digital “fire alarm” for mental distress. New York Times. 2019.
13. Akili. https://www.akiliinteractive.com.
14. Kollins SH, DeLoss DJ, Canadas, E, et al. A novel digital intervention for actively reducing severity of paediatric ADHD (STARS-ADHD): a randomised controlled trial. Lancet Digital Health. 2020;2:E168-E178.
15. Hays S. Approaching 1000 Mental Health Startups in 2020. https://medium.com/what-if-ventures/approaching-1-000-mental-health-startups-in-2020-d344c822f757.
16. Szaley J. The Renaissance: The Rebirth of Science and Culture. Live Science. 2016. https://www.livescience.com/55230-renaissance.html.
17. Eyre HA, Ellsworth W, Fu E, et al. Responsible innovation in mental health. Lancet Psychiatry. 2020; (In press).
18. Fernandes BS, Williams LM, Steiner J, et al. The new field of precision psychiatry. BMC Med. 2017;15:80.
19. Brady L, Hotopf M, Broekmans A, et al. Remote assessment of disease and relapse in major depressive disorder (RADAR-MDD). https://fnih.org/sites/default/files/final/pdf/CS5_RADAR%20MDD.pdf.
20. Affectiva. https://www.affectiva.com.
21. Jain FA, Walsh RN, Eisendrath SJ, et al., Critical analysis of the efficacy of meditation therapies for acute and subacute phase treatment of depressive disorders: a systematic review. Psychosomatics. 2015;56:140-152.
22. Cramer H, Lauche R, Langhorst J, Dobos G. Yoga for depression: a systematic review and meta-analysis. Depress Anxiety. 2013;30:1068-1083.
23. Laird K, Jain F, Lavretsky H. Convergence neuroscience of meditative mind-body therapies for mental health. Eyre HA, Lavretsky H, Reynolds III C2020, Eds. Convergence Mental Health: A Roadmap Towards Transdisciplinary Innovation. New York City: Oxford University Press; 2020.
24. Eyre HA, Robb A, Abbott R, Hopwood M. Mental health innovation diplomacy: an under-recognised soft power. Aust N Z J Psychiatry. 2019;53:474-475.
25. Psychiatric Cell Map Initiative 01/25/20; Available from: https://pcmi.ucsf.edu.
26. Mind O. Health Brains Financing Initiative. https://onemind.org/healthy-brains-financing-initiative.
27. Smith E, Au R, Mosse M, et al. Rebooting late-life mental health innovation and entrepreneurship with convergence science. Am J Geriat Psychiatry. 2020; In Press.❒
Newsletter
Receive trusted psychiatric news, expert analysis, and clinical insights — subscribe today to support your practice and your patients.