News
Article
Get Cozy and Keep Sleeping
Author(s):
Here’s how we can help improve quality of sleep in both our patients and ourselves.
DavidPrado_AdobeStock

AMERICAN ASSOCIATION FOR PSYCHIATRIC ADMINISTRATION AND LEADERSHIP
Sleep. It is a natural part of our existence, like breathing or eating. Almost everyone knows how it feels to have a good night’s rest. In psychiatry, we are all too aware that sleep fluctuations can be an indication of mental health changes. We have become so used to our patients saying, “I can’t sleep” or “I’m so tired all the time.” Many psychiatrists have their go-to hypnotic medications for times like these. But we also know patients who do not obtain relief from a trazodone or z-drug prescription.
The American Academy of Sleep Medicine practice guidelines are clear that all pharmacological agents, including over-the-counter medications, either were deemed weak in efficacy or had adverse effects that outweighed the benefits.1 Although the gold standard treatment is cognitive behavioral therapy for insomnia (CBTi), this can be a cost- and access-prohibitive option in most locations.1
The following is a patient encounter that both helped me reflect on how to improve conversations surrounding sleep and led me to reassess my own sleep habits.
“Mrs K” was a 47-year-old female seeing me in follow-up for both major depressive disorder and generalized anxiety disorder. She started seeing me a year ago after her husband’s death from cancer. She has been undergoing monthly psychotherapy and has been effectively managed on escitalopram 10 mg daily monotherapy.
On this visit, her primary concern was that she could not sleep. We had tried several pharmacologic options, from over-the-counter melatonin to prescription antihistaminergics to even the newer dual orexin receptor antagonists. I felt helpless and somewhat frustrated that she just could not sleep. I could feel the imposter syndrome trickling in as I thought, “Is this a reflection of my abilities?”
Just as we all have experienced feeling well rested, nearly all of us have also experienced the impact of a night spent tossing and turning and the subsequent effects on next-day performance. Chronic insomnia is defined as having 1 or more qualitative sleep difficulty associated with more than 1 daytime symptom occurring ≥ 3 nights per week for > 3 months.2 This affects anywhere from 9% to 15% of the general population.3
Patients like Mrs K, whose sleep remains an ongoing primary concern despite the improvement of other psychiatric symptoms, can be a challenge for us in psychiatry. Our toolbox usually includes asking about activities prior to bedtime, such as blue light exposure, physical activity, and food intake. We also ask about their sleep schedule, including naps. One aspect we may overlook, however, is asking patients about their bed environment, in detail.
I discussed the usual “sleep hygiene” with Mrs K. She described her daily 30-minute walks around the neighborhood and the Mediterranean diet that she implemented decades ago. She routinely eats 2 hours before bedtime and does not have a sweet tooth. She drinks 1 cup of coffee in the mornings and has a strict bedtime and wake time, even on the weekends. She heads to bed around midnight, tossing and turning nightly until she falls asleep.
She naturally wakes up at 7 AM but never feels like she slept well. She does not take naps. She denied symptoms of sleep apnea such as snoring, daytime sleepiness, and waking up gasping or choking. She is not much for cell phones and tablets but watches the news in the living room after breakfast. She is an avid reader and has a “reading chair” next to her bed. Her stress levels were “low, except for the fact that I can’t sleep!” She was doing all the right things.
Just when I thought there was nothing more to discuss but a referral to sleep medicine and a handout on CBTi resources Mrs K said, “It’s been so nice to have Mr Pickles with me. He keeps me active.” Mr Pickles was her 10-year-old Shih Tzu. It turns out that ever since her husband passed away, Mrs K had been allowing Mr Pickles to sleep in bed with her for company. She denied that Mr Pickles disturbs her sleep but mentioned that “he just loves to cuddle.”
We discussed a trial of keeping Mr Pickles out of her bed for 1 week to see if her sleep improved. Three months later, Mrs K returned for follow-up, beaming with a smile on her face. “I haven’t had Mr Pickles in bed with me since the last time I saw you! I don’t know why but I’m sleeping so much better!”
As our brain transitions through the stages of sleep, there is a constant check-in on the surroundings to ensure safety—a survival mechanism inherited from our ancestors. However, any minor sound, movement, or even brief light exposure can cause our brain to become aroused, just enough to double-check that our surroundings are still safe enough to continue sleeping.4,5
Most of the time, we have no awareness of these unconscious check-ins, with increased k-complexes when connected to polysomnography the only evidence something amiss may have even occurred.5 But with enough minor stimulation, you can end up with poorer quality sleep without even realizing it.
The bedroom environment is something that is underemphasized in our education. Everything from room temperature to the dim streetlight through your window to the texture of the blankets can significantly affect your sleep quality.6,7 Perhaps being cozy is synonymous with feeling safe for our brains.
For Mrs K, it appeared that Mr Pickles initially provided an emotional comfort and safety mechanism after her husband’s passing as she would fall asleep. Over time, though, the increased subconscious vigilance of having Mr Pickles in bed began to offset that perceived benefit and eventually became the source of Mrs K’s problem. Despite no longer keeping Mr Pickles in her bed, Mrs K realized that she could still obtain the same emotional comfort from her dog as long as his bed was next to her bed.
Ever since this case, I have become more curious about my own bed environment and how to optimize my sleep. If we are going to tell patients how important sleep is for their mental health, we should practice what we preach. As the Table6,7 shows, there are numerous environmental factors that affect our sleep outside of a psychiatric diagnosis.
Table. Sleep Environment Tips6,7
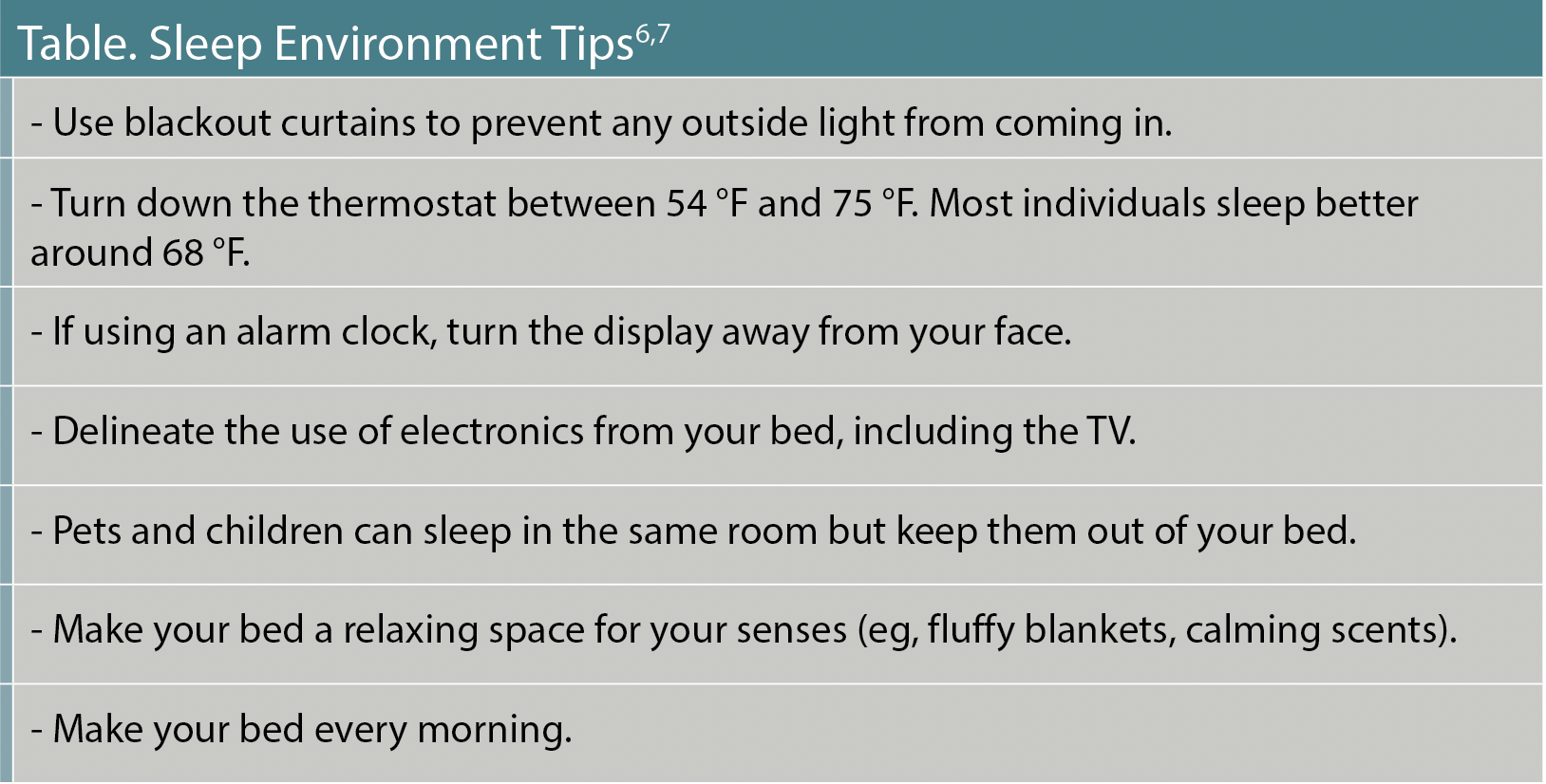
This may seem simple, intuitive, and elementary, but how many of us can truly say that we follow every single one of these points? Like many things in life, small changes over time can result in sustained habits rather than trying to shift everything all at once.
I have always gone to bed fairly early (8:30 PM) and woken before sunrise (4 AM). Falling asleep has not been an issue for me since high school. I would usually play a few puzzle games on my phone in bed and turn off the lights by 9 PM. In the mornings, I would scroll through any email, texts, and social media updates I may have missed overnight. At least once a week, I would find myself scrolling for over an hour before getting out of bed to start my day, and on those days, I would feel sluggish.
For the past several months, I made the conscious decision to avoid using my phone or laptop while my body is physically touching my bed. If I wanted to check an email in the morning, I would force myself to get out of bed to start the day first.
On the first night of no electronics in bed, I realized that my mind was unusually racing with thoughts. It dawned on me that part of my nightly ritual had been to mentally wind down by focusing my mind on puzzles on my phone. To combat this on night 2, I took a book of sudoku and a pencil into bed with me. It worked. I fell asleep as easily as I always had.
In the morning, although it was a challenge, I refused to touch my phone until I was physically out of bed. After brushing my teeth and putting on my watch, I finally picked up my phone and walked over to the kitchen to make some tea. Surprisingly, the most significant impact was not the decrease in electronic use before falling asleep, but rather the positive change in efficiency and energy throughout the day by not touching my phone until I am out of bed every morning.
In light of the upcoming Sleep Awareness Week and World Sleep Day on March 15, 2024, I encourage all my clinician colleagues to commit to 1 sleep environment change over the next month and observe how your sleep and wakefulness qualities change. Perhaps you will not notice anything change and will rest easy in the validation that your sleep is at peak quality. Or perhaps you will notice an improvement in your daily performance. Either way, the wonderful thing about sleep health is that we get to practice it every night because sleep will eventually happen for us all.
Dr Tomatsu is chief resident at the Atrium Health Sandra and Leon Levine Psychiatry Residency Program at Behavioral Health Charlotte. She will be joining the Center for Circadian and Sleep Medicine at Northwestern University this year as a fellow in sleep medicine.
References
1. Sateia MJ, Buysse DJ, Krystal AD, et al. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13(2):307-349.
2. American Academy of Sleep Medicine. International Classification of Sleep Disorders, third edition (ICSD-3). American Academy of Sleep Medicine; 2014.
3. Edinger JD, Means MK. Cognitive-behavioral therapy for primary insomnia. Clin Psychol Rev. 2005;25(5):539-558.
4. Tamaki M, Sasaki Y. Surveillance during REM sleep for the first-night effect. Front Neurosci. 2019;13:1161.
5. Cash SS, Halgren E, Dehghani N, et al. The human K-complex represents an isolated cortical down-state. Science. 2009;324(5930):1084-1087.
6. Harvey AG, Buysse DJ. Treating Sleep Problems: A Transdiagnostic Approach. The Guilford Press; 2018.
7. Bootzin RR, Perlis ML. Sleep hygiene. In: Perlis ML, Aloia M, Kuhn B, Eds. Behavioral Treatments for Sleep Disorders: A Comprehensive Primer of Behavioral Sleep Medicine Interventions. Academic Press; 2011.
Newsletter
Receive trusted psychiatric news, expert analysis, and clinical insights — subscribe today to support your practice and your patients.





