CME
Article
Psychiatric Times
Serotonin Reuptake Inhibitor and Bleeding Risk, Part 2: Gastrointestinal (GI) Bleeding, Malignancy, Pregnancy, and Surgical Considerations
Author(s):
In this CME article, review literature on SRI-related bleeding complications in patients with GI bleeding, malignancy, perioperative settings, pregnancy, and hormonal therapy.
SciePro/AdobeStock

CATEGORY 1 CME
Premiere Date: October 20, 2023
Expiration Date: April 20, 2025
This activity offers CE credits for:
1. Physicians (CME)
2. Other
All other clinicians either will receive a CME Attendance Certificate or may choose any of the types of CE credit being offered.
ACTIVITY GOAL
The goal of this activity is to describe current understanding of bleeding risk associated with use of serotonin reuptake inhibitors (SRIs) and to review research-informed literature on related bleeding complications in patients with gastrointestinal (GI) bleeding risk, malignancy, in perioperative settings, pregnancy, and in context of hormonal therapies.
LEARNING OBJECTIVES
After engaging with the content of this CME activity, you should be better prepared to:
- Review literature on SRI-related bleeding complications in patients with GI bleeding, malignancy, perioperative settings, pregnancy, and hormonal therapy.
- Describe potential interventions to mitigate the risk of SRI-related bleeding complications.
TARGET AUDIENCE
This accredited continuing education (CE) activity is intended for psychiatrists, psychologists, primary care physicians, physician assistants, nurse practitioners, and other health care professionals who seek to improve their care for patients with mental health disorders.
ACCREDITATION/CREDIT DESIGNATION/FINANCIAL SUPPORT
This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of Physicians’ Education Resource,® LLC, and Psychiatric Times.® Physicians’ Education Resource, LLC, is accredited by the ACCME to provide continuing medical education for physicians.
Physicians’ Education Resource, LLC, designates this enduring material for a maximum of 1.5 AMA PRA Category 1 Credits.™ Physicians should claim only the credit commensurate with the extent of their participation in the activity.
This activity is funded entirely by Physicians’ Education Resource, LLC. No commercial support was received.
OFF-LABEL DISCLOSURE/DISCLAIMER
This accredited CE activity may or may not discuss investigational, unapproved, or off-label use of drugs. Participants are advised to consult prescribing information for any products discussed. The information provided in this accredited CE activity is for continuing medical education purposes only and is not meant to substitute for the independent clinical judgment of a physician relative to diagnostic or treatment options for a specific patient’s medical condition. The opinions expressed in the content are solely those of the individual faculty members and do not reflect those of Physicians’ Education Resource, LLC.
FACULTY, STAFF, AND PLANNERS’ DISCLOSURES AND CONFLICT OF INTEREST (COI) MITIGATION
None of the staff of Physicians’ Education Resource, LLC, or Psychiatric Times or the planners or the authors of this educational activity have relevant financial relationship(s) to disclose with ineligible companies whose primary business is producing, marketing, selling, reselling, or distributing health care products used by or on patients.
For content-related questions, email us at PTEditor@mmhgroup.com; for questions concerning the accreditation of this CME activity or how to claim credit, please contact info@gotoper.com and include “Serotonin Reuptake Inhibitor and Bleeding Risk: A Practical Review for the Consultation Psychiatrist, Part 2 of 2: Gastrointestinal (GI) Bleeding, Malignancy, Pregnancy, and Surgical Considerations” in the subject line.
HOW TO CLAIM CREDIT
Once you have read the article, please use the following URL to evaluate and request credit: https://education.gotoper.com/activity/ptcme23oct. If you do not already have an account with PER,® you will be prompted to create one. You must have an account to evaluate and request credit for this activity.
Serotonin reuptake inhibitors (SRIs), including selective SRIs (SSRIs) and other psychotropic medications, are used to treat a variety of psychiatric conditions, including many mood and anxiety disorders. They are among the most frequently prescribed medications in the United States. SSRIs are the most prescribed type of SRIs and were initially heralded as a safer, easier alternative to earlier psychiatric medications used for the same indications. A growing body of literature has elucidated potential adverse effects that appear germane to all medications that inhibit serotonin reuptake.
One example of this is SRI-related increases in bleeding risk. Even though the presence of this risk is becoming more widely accepted and known by clinicians, the literature—which is simultaneously complex and limited—is not always easily translated into clinical practice. In this 2-part series, we aim to address this problem by offering a summary of the current state of the literature on the risk of SRI-related bleeding and offer advice for clinical practice.
In part 1, we reviewed physiological mechanisms by which SRIs can increase bleeding risk,1 including major findings on the risk of SRI-related bleeding across a variety of cardiovascular conditions and blood-thinning agents. Our recommendation was that clinicians should take an individualized approach to managing SRIs in these circumstances rather than using “rules of thumb.”
Here in part 2, we will describe bleeding risk with SRIs in gastrointestinal (GI) bleeds, surgical/perioperative conditions, malignancy, and pregnancy, and in patients treated with hormonal therapies. We will offer recommendations that may have broader applicability in patients who are taking SRIs, such as using gastroprotective agents when an SRI is continued in a patient who is at an elevated risk for bleeds, and factoring in medication interactions when deciding how to manage an SRI in medically complex patients.
As noted in part 1, we use the general term SRI (serotonin reuptake inhibitor) for any medication with this property, which can include SSRIs, SNRIs, tricyclic antidepressants, and more. When cited studies examined 1 medication or class of medications, we have attempted to specify this in the text.
GI Bleeding
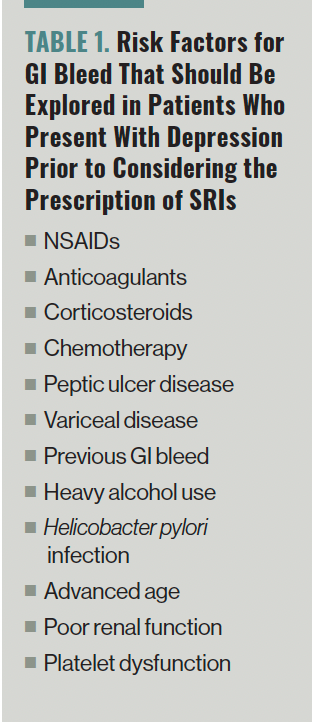
The bidirectional signaling between the gut and brain has become a focus of research over recent decades, with an expanding body of literature demonstrating a link between mental and GI health.2-5 Despite the additive risk of GI bleeding from the combination of SRIs with nonsteroidal anti-inflammatories (NSAIDs) or warfarin,1 the potential for SRIs to further increase the risk of GI bleeding when prescribed with other ulcer-causing medications has been underexplored in the literature.6 The risk factors for GI bleeding should be evaluated in patients who present with depression prior to the prescription of SRIs (Table 1).
Table 1. Risk Factors for GI Bleed That Should Be Explored in Patients Who Present With Depression Prior to Considering the Prescription of SRIs
Peptic ulcer disease (PUD) is a common cause of GI bleeding.7 Perforated peptic ulcers are associated with high mortality, rising to nearly 50% in the setting of advanced age.8 In 1 large Taiwanese study, the incidence of PUD in patients with depression was twice as high as those without (33.2 vs 16.8 per 1000 person-years), with an age adjusted HR of 1.97 (95% CI, 1.89-2.06).9 Another large longitudinal cohort study showed a significant bidirectional relationship between depression and PUD compared to controls (P < .001 for PUD in patients with depression, and P < .001 for depression in patients with PUD) after adjusting for lifestyle and environmental factors.10,11 Robust data from a recent population-based study of 83.9 million person-years further support the association between PUD and depression.11 In a study of 337,536 UK Biobank participants, the authors concluded there was a causal link between depression and various GI illnesses, including GI hemorrhage (OR 1.26; 95% CI, 1.11-1.43).12,13
The potential for GI bleeding in patients with comorbid depression and heavy alcohol use should be considered by prescribers. Heavy alcohol use, especially distilled spirits, contributes to PUD and that effect is amplified with concomitant NSAID use.14 Alcohol can specifically contribute to development of cirrhosis, in turn causing thrombocytopenia and variceal disease, which are both major risk factors for GI bleeding. Individuals with alcohol dependence are 3.7 times more likely to have major depression and 2.8 times more likely to have dysthymia—therefore, they may present requesting antidepressant treatment.15
The relationship between alcohol and depression has been underappreciated as a potential confounder in studies seeking to calculate the risk of GI bleeding in the setting of SRI use. For example, Opatrny and colleagues found that the addition of alcohol abuse as a novel covariate reduced the size of the associations observed between antidepressant use and GI bleeding.16 More research is needed to further characterize these interactions.
Clinicians should encourage patients to view reduction of alcohol use as an important step in treating anxiety and depression. The evidence for the use of SRIs in alcohol-induced psychiatric conditions is sparse and continued alcohol use likely blunts their efficacy. In rare instances, SSRIs may lead to increased alcohol consumption as an adverse effect.17
Gastroprotection from acid-suppressing medications may reduce the risk of GI bleed in patients taking SRIs.18,19 Gastroprotection should be considered for individuals for whom SRI prescription is justified despite the presence of risk factors for GI bleeding, particularly those using coprescribed NSAIDs or warfarin, and is supported by an emerging body of literature.6,18-21 As many as 80% of patients who develop upper GI bleeding due to PUD are on 1 or more medications known to increase the risk of PUD or GI bleeding, and the utilization of gastroprotection is low at 8.5%.22
Clinicians should check for drug-drug interactions when adding gastroprotective agents, as several proton pump inhibitors (PPIs) and H2 blockers can alter serum levels of SRIs through effects on the cytochrome system in the liver. A 50% dose reduction of escitalopram should be considered when coprescribed with omeprazole or esomeprazole.23 Electrocardiographic monitoring of the QTc interval should be performed in patients coprescribed a QTc-prolonging antidepressant and cimetidine.24
Malignancy
Depressive symptoms are the most common psychiatric sequelae of oncologic illness and antidepressants are the most commonly prescribed psychotropic medication in this population.25,26 Malignancy is generally regarded as a prothrombotic state, largely due to aberrant proteins associated with malignant cells interacting with blood vessels and inducing the coagulation cascade. However, malignancy is often accompanied by numerous factors associated with an increased risk of bleeding, including disruption of the integrity of healthy tissue by the tumor, platelet, or bone marrow dysfunction secondary to chemotherapy or other therapeutics, or anticoagulation therapy prescribed for cancer-related thromboembolic disease. Severe thrombocytopenia is a common adverse effect of cancer treatments that is associated with bleeding events.
Despite this, the literature on antidepressants and bleeding in oncologic patients is meager. One of the few studies on bleeding risk and SRI use in patients with malignancy found that patients on SSRIs who underwent surgery for breast cancer had increased rates of reoperation due to postoperative bleeding, with an adjusted relative risk of 2.3 compared to non-SSRI users.27 Given that the focus of this study was on surgical procedures and outcomes, it is difficult to ascertain what conclusions can be drawn on the contribution of the malignancy itself to the study’s findings. This illustrates the paucity of literature on SRI-associated bleeding in risk in patients with malignancy.
The principles outlined in prior sections, such as being cautious when coprescribing antidepressants and warfarin, NSAIDs, or antiplatelet agents, should be used to guide clinicians when caring for oncologic patients. Given the high burden of psychiatric illness in patients with cancer, the authors recommend prescribing SRIs for patients with malignancy for whom these medications would otherwise be indicated unless the patient has additional risk factors such as severe thrombocytopenia or active bleeding.
Surgical and Perioperative Care
The question of when to suspend and restart SRIs perioperatively frequently arises in hospital settings. Available data regarding bleeding risk with SRI use in this context are highly variable and dependent on the specific procedure, coprescribed agents, and patient characteristics. Studies on bleeding risk and SRIs, organized by procedure type, are summarized in Table 1 in part 1 of our series.1
There is a modest association between SRI use and increased risk of certain perioperative and postoperative complications, including increased risk of bleeding requiring blood transfusions, hospital readmissions, and mortality.28-30 Most of these studies in this domain are observational or case-control in design, have mixed results, and are difficult to apply to individual patients.
In 1 review, 7 of 10 studies reported no significant difference in mortality, and 5 of 7 showed no difference in risk of bleeding.31 Another observational study that examined the rate of perioperative complications in more than 500,000 patients who were prescribed SSRIs at more than 375 hospitals found an increased risk of bleeding (OR, 1.09; NNH, 424), higher mortality (OR, 1.2; NNH, 839), and increased risk of readmission within 30 days (OR, 1.22; NNH, 75) in the SSRI population, regardless of surgery type or concomitant use of anticoagulants.32
It is not clear from these observational studies whether SRIs themselves are responsible for the higher rates of complications or whether the higher rates are due to confounding factors. For example, in the above study, the patients taking SSRIs were found to have higher rates of comorbid medical illnesses associated with worse surgical outcomes, including chronic obstructive pulmonary disease (COPD) and obesity.32
One retrospective matched-cohort study found that preoperative SRI use was associated with increased risk of requiring a blood transfusion postoperatively, but only in the first 24 hours after surgery. Patients who resumed SRI use in the 72 hours after surgery did not have an increased risk of requiring a blood transfusion and were significantly less likely to require transfusion than patients who restarted later or not at all (43.2% vs 60.3%, respectively).33 Taken together, these results suggest that, although preoperative SRI use may predispose patients to adverse bleeding in the brief window directly after surgery, restarting SRIs after surgery is likely safe.
When examining specific perioperative circumstances, higher rates of intraoperative blood loss and increased rates of blood transfusion have been observed in patients who underwent various orthopedic surgeries and concomitantly took SRIs.30,34 For cardiac procedures, a meta-analysis of observational studies in coronary artery bypass graft (CABG) surgery in patients taking SSRIs showed an increased risk of transfusion but without increased risk of mortality.35 These findings led the investigators to recommend continuing SRI use prior to elective procedures.36 One study that examined smaller, elective, or nonvascular procedures described a significantly increased risk that patients taking SSRIs will require reoperation due to bleeding,27 while a dental study reported no increased risk of bleeding during tooth extractions for patients who are taking SSRIs.37
Decisions about withholding SRIs are further complicated by characteristics of individual agents. Medications with short half-lives, such as venlafaxine and paroxetine, are fully excreted within days (with a concomitant increased risk of discontinuation syndrome), whereas SRIs with longer half-lives, such as fluoxetine, require weeks to be excreted. Additionally, different SRIs have variable CYP450 enzyme inhibition profiles and differing impacts on serum levels of other medications the patient is taking.
In summary, patients taking SRIs preoperatively have a small increased risk of perioperative complications (specifically, increased bleeding and requiring transfusions intra- or postoperatively), but the absolute risk appears to be small and unlikely to be clinically significant for most patients. The available limited data do not support the suspension of SRIs post- or perioperatively. The concern for SRI-induced surgical bleeding should be limited to those patients who have existing hematologic concerns, such as severe thrombocytopenia or von Willebrand disease; those who are coprescribed NSAIDS, antiplatelet agents, or warfarin; and those who are undergoing a procedure with a high risk of intraoperative blood loss.
Pregnancy
Pregnancy is a period of increased risk for both depression and anxiety.38,39 Untreated depression during pregnancy is associated with negative fetal and maternal outcomes in pregnancy, childbirth, and the postpartum period, including development of the newborn. Examples include increased likelihood of preterm birth and preeclampsia for the mother, and low birth weight and elevated risk for psychiatric disorders in the offspring.40-43
SRIs are the first-line antidepressant medications in pregnancy and the peripartum period due to their favorable safety profile in pregnancy. Sertraline is considered the preferred agent during pregnancy and breastfeeding, while paroxetine is associated with a slight increased risk of teratogenicity. Matching overall trends in the general population over the last several decades, the use of SRIs in the pregnant/peripartum population has increased in recent years.44
From implantation to parturition, pregnancy is accompanied by a multitude of physiological changes that alter hemostasis. These include placental embedding into the uterine wall, a 10% decrease in platelet count, complex and often drastic changes in clotting factors, and large shifts in hormones (eg, estrogen, progesterone) that increase the risk of thrombi or otherwise affect coagulability and the vasculature.45-47 Although most of these changes are pro-coagulative, some of the most feared complications of pregnancy involve high-volume blood loss, including ectopic pregnancy, placenta accreta or previa, and postpartum hemorrhage (PPH). PPH, in particular, is 1 of the major causes of maternal mortality and morbidity related to pregnancy and has increased in prevalence in recent years.38,48-50
Evidence for increased risk of bleeding in pregnant patients who are taking SRIs is conflicting. In an analysis of data from the US Food & Drug Administration (FDA) Adverse Events Reporting System, SRI use in pregnancy was tolerated well and not associated with increased risk of PPH.38 In a 2014 cohort study of more than 57,000 Norwegian women, no association was found between antidepressant use in pregnancy and obstetric hemorrhage.51 Nevertheless, a 2016 systematic review published results indicating that the odds for developing PPH were 1.32-fold higher (95% CI, 1.17-1.48) in antidepressant users (of both SRIs and non-SRIs) compared with individuals who had not taken antidepressants.52 The authors of a 5-year Swedish cohort study also concluded that SSRI use in pregnancy was associated with increased risk of both PPH and postpartum anemia. A Swedish register-based study of more than 31,000 pregnant women found that those who took SSRIs during their pregnancy were 34% more likely to have PPH.53
Although SRIs are generally safe in pregnancy, the available data suggest that there is likely to be an increased risk of PPH and other adverse bleeding-related events; however, the absolute risk remains low. This is just one of many factors that should be considered when deciding to start, restart, dose-reduce, or stop antidepressants in pregnancy. Other factors are listed in Table 2. The informed psychiatric clinician should work with each patient to help them understand the most salient factors to consider and collaborate on an optimal treatment plan tailored to the individual patient.
Table 2. Factors to Consider When Deciding to Start, Restart, Dose- Reduce, or Stop Antidepressants During Pregnancy

Hormonal Therapy
Estrogen-based hormone replacement therapy (HRT) is commonly prescribed in postmenopausal and perimenopausal women, and it is a part of gender-affirming hormone therapy (GAHT) in transfeminine individuals. All estrogen preparations are associated with an increased risk of thrombosis and hypercoagulability, although the risk appears to be lower for preparations that are administered transdermally.54-56 Notably, higher thrombosis risk likely means lower bleeding risk overall, but it may also portend a higher risk of exposure to anticoagulant agents as described in part 1 of our series.1
SRIs are commonly used in postmenopausal women for both psychiatric and menopause-related indications (namely, the management of hot flashes).57-60 Research suggests that post- and perimenopausal individuals with depression who are receiving both HRT and treatment with SSRIs experience an improved quality of life when compared with individuals who are receiving treatment with SSRIs alone.61 In gender-affirming care, SRI antidepressants are also a commonly coprescribed class of medication with GAHT.62,63
Despite these associations, the investigators were unable to find any research specific to bleeding events in patients taking both SRI antidepressants and HRT/GAHT. More research is required to direct clinicians regarding the use of SRIs and the risk of bleeding in individuals who receive HRT/GAHT. Testosterone-based GAHT for transmasculine individuals also carries risks, notably polycythemia and liver disease, although bleeding appears to be a less common concern.
Concluding Thoughts
SRIs are commonly prescribed medications in many clinical situations. SRIs carry a slightly increased risk in bleeding due to their inhibition of platelet aggregation and vasoconstriction, both of which facilitate clotting. Although this effect is negligible and clinically insignificant for most patients, it may be relevant for patients with other medical or surgical illness depending on the specific illness, associated procedures, or coprescribed medications. The informed clinician will soon find that the literature on SRI-induced bleeding is limited and requires interpretation for each individual to evaluate the impact of any other medical conditions or polypharmacy that influences their overall bleeding risk.
Several take-home points are clinically noteworthy. Coprescribing an acid-suppressing agent plus an SRI can decrease the risk of GI bleeding in patients who also take antiplatelet agents or NSAIDs. Data are insufficient to consider dose adjustment or discontinuation of SRI therapy in patients undergoing emergent, minor, or elective procedures, and in those receiving heparin products or novel anticoagulant medications. Patients who receive SRIs are more likely to require blood transfusions during or immediately following major or vascular surgical procedures. It is unclear whether transfusions or SRI use contribute to poorer outcomes or higher mortality. It is also unclear whether stopping SRIs prior to these procedures reduces the risk of bleeding.
It is important to consider the precipitation of SRI withdrawal syndromes, especially for shorter-acting SRI agents, that can occur with abrupt discontinuation of an SRI. The elimination of drug-drug interactions after SRI discontinuation may require dose adjustment of other interacting drugs. Future research would be helpful to guide safe clinical prescription of SRIs or other antidepressants in patients with malignancy, critical illness, or organ failure.
Dr Robbins-Welty is chief resident of the combined Internal Medicine & Psychiatry residency program in the departments of medicine and psychiatry at Duke University Medical Center in Durham, North Carolina. Dr Tuck is a medical instructor in the department of psychiatry and behavioral sciences at Duke University Medical Center.
Dr Marchant is affiliated with the department of psychiatry at Westmead Hospital and the department of consultation-liaison psychiatry at Concord Repatriation General Hospital in Sydney, Australia. Dr Gleason is affiliated with the Department of Consultation-Liaison Psychiatry at Concord Repatriation General Hospital and the Florey Institute of Neuroscience and Mental Health at the University of Melbourne in Melbourne, Australia. Dr Key is an assistant professor in the department of psychiatry & behavioral sciences; a courtesy assistant professor in the department of oncology; and program director of the consultation-liaison psychiatry fellowship at the University of Texas at Austin Dell Medical School in Austin, Texas. Dr Lubrano di Ciccone is an associate professor in the department of behavioral medicine at Moffitt Cancer Center in Tampa, Florida. Dr Chopra is affiliated with the University of Texas MD Anderson Cancer Center in Houston, Texas. Dr Mojtahedzadeh is affiliated with the department of psychiatry and Simms/Mann-UCLA Center for Integrative Oncology at the University of California, Los Angeles, in California. Dr Fonseca is a fellow in consultation-liaison psychiatry at the Mayo Clinic in Rochester, Minnesota. Dr Amonoo is an assistant professor of psychiatry at Brigham and Women’s Hospital in Boston, Massachusetts. Dr DeSimone is a clinical assistant professor at Philadelphia College of Osteopathic Medicine and a consultation-liaison psychiatrist at Bayhealth Medical Center in Dover, Delaware. Dr McFarland is an associate professor in the departments of psychiatry and medicine at the Wilmot Cancer Centre of the University of Rochester Medical Center in Rochester, New York.
References
1. Robbins-Welty GA, Tuck AN, Marchant D, et al. Bleeding risk with SSRIs: part 1: cardiovascular and cerebrovascular considerations. Psychiatric Times. 2023;40(9):35-39.
2. Mayer EA. Gut feelings: the emerging biology of gut-brain communication. Nat Rev Neurosci. 2011;12(8):453-466.
3. Breit S, Kupferberg A, Rogler G, Hasler G. Vagus nerve as modulator of the brain-gut axis in psychiatric and inflammatory disorders. Front Psychiatry. 2018;9:44.
4. Furness JB. The enteric nervous system and neurogastroenterology. Nat Rev Gastroenterol Hepatol. 2012;9(5):286-294.
5. Mayer EA. The neurobiology of stress and gastrointestinal disease. Gut. 2000;47(6):861-869.
6. Scarpignato C, Gatta L, Zullo A, Blandizzi C; SIF-AIGO-FIMMG Group; Italian Society of Pharmacology, the Italian Association of Hospital Gastroenterologists, and the Italian Federation of General Practitioners. Effective and safe proton pump inhibitor therapy in acid-related diseases - a position paper addressing benefits and potential harms of acid suppression. BMC Med. 2016;14(1):179.
7. Wuerth BA, Rockey DC. Changing epidemiology of upper gastrointestinal hemorrhage in the last decade: a nationwide analysis. Dig Dis Sci. 2018;63(5):1286-1293.
8. Christensen S, Riis A, Nørgaard M, et al. Short-term mortality after perforated or bleeding peptic ulcer among elderly patients: a population-based cohort study. BMC Geriatr. 2007;7:8.
9. Hsu CC, Hsu YC, Chang KH, et al. Depression and the risk of peptic ulcer disease: a nationwide population-based study. Medicine (Baltimore). 2015;94(51):e2333.
10. Kim SY, Min C, Oh DJ, Choi HG. Reciprocal association between depression and peptic ulcers: two longitudinal follow-up studies using a national sample cohort. Sci Rep. 2020;10(1):1749.
11. Lee YB, Yu J, Choi HH, et al. The association between peptic ulcer diseases and mental health problems: a population-based study: a STROBE compliant article. Medicine (Baltimore). 2017;96(34):e7828.
12. Momen NC, Plana-Ripoll O, Agerbo E, et al. Association between mental disorders and subsequent medical conditions. N Engl J Med. 2020;382(18):1721-1731.
13. Mulugeta A, Zhou A, King C, Hyppönen E. Association between major depressive disorder and multiple disease outcomes: a phenome-wide Mendelian randomisation study in the UK Biobank. Mol Psychiatry. 2020;25(7):1469-1476.
14. Strate LL, Singh P, Boylan MR, et al. A prospective study of alcohol consumption and smoking and the risk of major gastrointestinal bleeding in men. PLoS One. 2016;11(11):e0165278.
15. McHugh RK, Weiss RD. Alcohol use disorder and depressive disorders. Alcohol Res. 2019;40(1):arcr.v40.1.01.
16. Opatrny L, Delaney JA, Suissa S. Gastro-intestinal haemorrhage risks of selective serotonin receptor antagonist therapy: a new look. Br J Clin Pharmacol. 2008;66(1):76-81.
17. Gimeno C, Dorado ML, Roncero C, et al. Treatment of comorbid alcohol dependence and anxiety disorder: review of the scientific evidence and recommendations for treatment. Front Psychiatry. 2017;8:173.
18. Targownik LE, Bolton JM, Metge CJ, et al. Selective serotonin reuptake inhibitors are associated with a modest increase in the risk of upper gastrointestinal bleeding. Am J Gastroenterol. 2009;104(6):1475-1482.
19. de Abajo FJ, García-Rodríguez LA. Risk of upper gastrointestinal tract bleeding associated with selective serotonin reuptake inhibitors and venlafaxine therapy: interaction with nonsteroidal anti-inflammatory drugs and effect of acid-suppressing agents. Arch Gen Psychiatry. 2008;65(7):795-803.
20. Paton C, Ferrier IN. SSRIs and gastrointestinal bleeding. BMJ. 2005;331(7516):529-530.
21. de Jong HJ, Korevaar JC, van Dijk L, et al. Suboptimal prescribing of proton-pump inhibitors in low-dose aspirin users: a cohort study in primary care. BMJ Open. 2013;3(7):e003044.
22. Romstad KK, Detlie TE, Søberg T, et al. Gastrointestinal bleeding due to peptic ulcers and erosions - a prospective observational study (BLUE study). Scand J Gastroenterol. 2020;55(10):1139-1145.
23. Gjestad C, Westin AA, Skogvoll E, Spigset O. Effect of proton pump inhibitors on the serum concentrations of the selective serotonin reuptake inhibitors citalopram, escitalopram, and sertraline. Ther Drug Monit. 2015;37(1):90-97.
24. FDA drug safety communication: revised recommendations for Celexa (citalopram hydrobromide) related to a potential risk of abnormal heart rhythms with high doses. FDA. Updated December 15, 2017. Accessed July 20, 2023. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-revised-recommendations-celexa-citalopram-hydrobromide-related
25. Anuk D, Özkan M, Kizir A, Özkan S. The characteristics and risk factors for common psychiatric disorders in patients with cancer seeking help for mental health. BMC Psychiatry. 2019;19(1):269.
26. Punekar RS, Short PF, Moran JR. Use of psychotropic medications by US cancer survivors. Psychooncology. 2012;21(11):1237-1243.
27. Gärtner R, Cronin-Fenton D, Hundborg HH, et al. Use of selective serotonin reuptake inhibitors and risk of re-operation due to post-surgical bleeding in breast cancer patients: a Danish population-based cohort study. BMC Surg. 2010;10:3.
28. Sajan F, Conte JV, Tamargo RJ, et al. Association of selective serotonin reuptake inhibitors with transfusion in surgical patients. Anesth Analg. 2016;123(1):21-28.
29. Mahdanian AA, Rej S, Bacon SL, et al. Serotonergic antidepressants and perioperative bleeding risk: a systematic review. Expert Opin Drug Saf. 2014;13(6):695-704.
30. Roose SP, Rutherford BR. Selective serotonin reuptake inhibitors and operative bleeding risk: a review of the literature. J Clin Psychopharmacol. 2016;36(6):704-709.
31. Sepehripour AH, Eckersley M, Jiskani A, et al. Selective serotonin reuptake inhibitor use and outcomes following cardiac surgery-a systematic review. J Thorac Dis. 2018;10(2):1112-1120.
32. Auerbach AD, Vittinghoff E, Maselli J, et al. Perioperative use of selective serotonin reuptake inhibitors and risks for adverse outcomes of surgery. JAMA Intern Med. 2013;173(12):1075-1081.
33. Wilson LB, Cox MR, Benns MV, et al. Serotonin-modulating antidepressants and risk of bleeding after trauma. Am Surg. 2018;84(11):1727-1733.
34. Movig KL, Janssen MW, de Waal Malefijt J, et al. Relationship of serotonergic antidepressants and need for blood transfusion in orthopedic surgical patients. Arch Intern Med. 2003;163(19):2354-2358.
35. Eckersley MJ, Sepehripour AH, Casula R, et al. Do selective serotonin reuptake inhibitors increase the risk of bleeding or mortality following coronary artery bypass graft surgery? A meta-analysis of observational studies. Perfusion. 2018;33(6):415-422.
36. Heimisdottir AA, Enger E, Morelli S, et al. Use of serotonin reuptake inhibitors is not associated with increased bleeding after CABG. Gen Thorac Cardiovasc Surg. 2020;68(11):1312-1318.
37. Napeñas JJ, Hong CH, Kempter E, et al. Selective serotonin reuptake inhibitors and oral bleeding complications after invasive dental treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112(4):463-467.
38. Perrotta C, Giordano F, Colombo A, et al. Postpartum bleeding in pregnant women receiving SSRIs/SNRIs: new insights from a descriptive observational study and an analysis of data from the FAERS Database. Clin Ther. 2019;41(9):1755-1766.
39. Hübner-Liebermann B, Hausner H, Wittmann M. Recognizing and treating peripartum depression. Dtsch Arztebl Int. 2012;109(24):419-424.
40. Pearlstein T. Depression during pregnancy. Best Pract Res Clin Obstet Gynaecol. 2015;29(5):754-764.
41. Ding XX, Wu YL, Xu SJ, et al. Maternal anxiety during pregnancy and adverse birth outcomes: a systematic review and meta-analysis of prospective cohort studies. J Affect Disord. 2014;159:103-110.
42. Guglielmi V, Vulink NC, Denys D, et al. Obsessive-compulsive disorder and female reproductive cycle events: results from the OCD and reproduction collaborative study. Depress Anxiety. 2014;31(12):979-987.
43. van der Waerden J, Galéra C, Larroque B, et al. Maternal depression trajectories and children’s behavior at age 5 years. J Pediatr. 2015;166(6):1440-8.e1.
44. Desaunay P, Eude LG, Dreyfus M, et al. Benefits and risks of antidepressant drugs during pregnancy: a systematic review of meta-analyses. Paediatr Drugs. 2023;25(3):247-265.
45. Bremme K, Ostlund E, Almqvist I, et al. Enhanced thrombin generation and fibrinolytic activity in normal pregnancy and the puerperium. Obstet Gynecol. 1992;80(1):132-137.
46. Ataullakhanov FI, Koltsova EM, Balandina AN, et al. Classic and global hemostasis testing in pregnancy and during pregnancy complications. Semin Thromb Hemost. 2016;42(7):696-716.
47. Ku DH, Arkel YS, Paidas MP, Lockwood CJ. Circulating levels of inflammatory cytokines (IL-1 beta and TNF-alpha), resistance to activated protein C, thrombin and fibrin generation in uncomplicated pregnancies. Thromb Haemost. 2003;90(6):1074-1079.
48. Lindqvist PG, Nasiell J, Gustafsson LL, Nordstrom L. Selective serotonin reuptake inhibitor use during pregnancy increases the risk of postpartum hemorrhage and anemia: a hospital-based cohort study. J Thromb Haemost. 2014;12(12):1986-1992.
49. van Stralen G, von Schmidt Auf Altenstadt JF, Bloemenkamp KW, et al. Increasing incidence of postpartum hemorrhage: the Dutch piece of the puzzle. Acta Obstet Gynecol Scand. 2016;95(10):1104-1110.
50. Knight M, Callaghan WM, Berg C, et al. Trends in postpartum hemorrhage in high resource countries: a review and recommendations from the International Postpartum Hemorrhage Collaborative Group. BMC Pregnancy Childbirth. 2009;9:55.
51. Lupattelli A, Spigset O, Koren G, Nordeng H. Risk of vaginal bleeding and postpartum hemorrhage after use of antidepressants in pregnancy: a study from the Norwegian Mother and Child Cohort Study. J Clin Psychopharmacol. 2014;34(1):143-148.
52. Jiang HY, Xu LL, Li YC, et al. Antidepressant use during pregnancy and risk of postpartum hemorrhage: a systematic review and meta-analysis. J Psychiatr Res. 2016;83:160-167.
53. Skalkidou A, Sundström-Poromaa I, Wikman A, et al. SSRI use during pregnancy and risk for postpartum haemorrhage: a national register-based cohort study in Sweden. BJOG. 2020;127(11):1366-1373.
54. Harper-Harrison G, Shanahan MM. Hormone replacement therapy. In: StatPearls. StatPearls Publishing; February 20, 2023.
55. Canonico M, Oger E, Plu-Bureau G, et al. Hormone therapy and venous thromboembolism among postmenopausal women: impact of the route of estrogen administration and progestogens: the ESTHER study. Circulation. 2007;115(7):840-845.
56. Winkler UH, Altkemper R, Kwee B, et al. Effects of tibolone and continuous combined hormone replacement therapy on parameters in the clotting cascade: a multicenter, double-blind, randomized study. Fertil Steril. 2000;74(1):10-19.
57. Bryant C, Judd FK, Hickey M. Anxiety during the menopausal transition: a systematic review. J Affect Disord. 2012;139(2):141-148.
58. Vesco KK, Haney EM, Humphrey L, et al. Influence of menopause on mood: a systematic review of cohort studies. Climacteric. 2007;10(6):448-465.
59. Mulhall S, Andel R, Anstey KJ. Variation in symptoms of depression and anxiety in midlife women by menopausal status. Maturitas. 2018;108:7-12.
60. Stubbs C, Mattingly L, Crawford SA, et al. Do SSRIs and SNRIs reduce the frequency and/or severity of hot flashes in menopausal women. J Okla State Med Assoc. 2017;110(5):272-274.
61. Jacobs PA, Hyland ME. An evaluation of the benefits of taking hormone replacement therapy with other prescription drugs. Maturitas. 2003;46(4):273-281.
62. Bränström R, Pachankis JE. Reduction in mental health treatment utilization among transgender individuals after gender-affirming surgeries: a total population study (published correction appears in Am J Psychiatry. 2020 Aug 1;177[8]:734). Am J Psychiatry. 2020;177(8):727-734.
63. Addis S, Davies M, Greene G, et al. The health, social care and housing needs of lesbian, gay, bisexual and transgender older people: a review of the literature. Health Soc Care Community. 2009;17(6):647-658.
Newsletter
Receive trusted psychiatric news, expert analysis, and clinical insights — subscribe today to support your practice and your patients.






