Case Scenario 2: Patient With Tardive Dyskinesia Prescribed a VMAT2 Inhibitor
In this custom video series, Leslie L. Citrome, MD, MPH, and Rose Mary Xavier, PhD, MS, RN, PMHNP-BC, review the case of a male patient with schizophrenia who develops symptoms of tardive dyskinesia and comments on the appropriateness for intervening with VMAT2 inhibitor therapy.
Episodes in this series

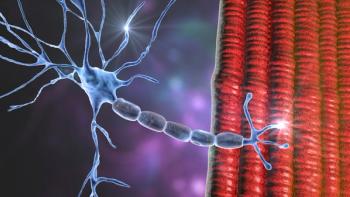
Leslie L. Citrome, MD, MPH: This is a 46-year-old man diagnosed with schizophrenia at age 25. He has been ill for over 20 years. He is currently on an oral atypical antipsychotic with a stable dose for the past 5 years. Any attempt to lower his atypical antipsychotic dosage results in early signs of relapse, in particular positive symptoms. His auditory hallucinations get worse. His paranoid delusions become more intense. His case manager noticed an increased frequency of unusual movements. Now this was not any of the rigidity and rhythmic tremor that he had long ago when he received haloperidol. This is different. This looks like piano playing movements of his hands. His hand, his fingers are moving as if they are playing the piano. It is not that rhythmic tremor that he used to have years ago. This kind of movement is unusual. He also has some shoulder shrugging, facial grimacing. And then the tongue is noticeable, it keeps on darting out of the mouth at random times like this. Now it is unusual, but we do see it with our patients. And sometimes we tend to ignore it, we sort of say well it is not really that noticeable. And we did it for a very long time, documented it but could not really do much about it. These movements are characteristic of classic tardive dyskinesia. Unfortunately for our case patient, he also noticed them and felt self-conscious. Now this is sometimes unusual for someone with schizophrenia to be insightful regarding their movements. We would expect to see that in someone with a mood disorder being more insightful about movements. But people with schizophrenia can also become aware of these movements, particularly when other people point them out. This resulted for this person to be more socially isolated. He was more anxious, and he was feeling a bit more paranoid relating to people looking at him. But you know what, people were not looking at him. And so that just fed into an ongoing paranoid delusion that he had any way. He felt people were staring at him. And to some degree they were. When someone sticks out their tongue, it is hard not to notice. He was on an antipsychotic regimen that needed some dose adjustments for him to have better control over his positive symptoms of schizophrenia. Ultimately, there was no other way of altering his medicines. And the TD [tardive dyskinesia] was diagnosed, it was there. And what can we do? Well, we can add a VMAT2 inhibitor. And actually, that is what was done. And his movements did improve, and he was able to be maintained on his antipsychotic regimen, and his positive psychotic symptoms were better managed. Dr. Xavier, what is your overall impression of this? Is this unusual, strange, or is it kind of a typical case?
Rose Mary Xavier, PhD, MS, RN, PMHNP-BC: Well, we cannot really say that it is unusual because we know that with any type of antipsychotic medication, which belongs to the category of dopamine blocking agents, the risk of tardive dyskinesia is there. Given his history, he has been diagnosed with schizophrenia since the age of 25. It is very likely that he was started on medications, an antipsychotic medication, and he has been treated with the same medication for about 5 years. The movements that you have described about this case are classic movements of tardive dyskinesia. The chorea, the athetoid movements, the tongue protrusion, the shoulder shrugging, the facial grimacing, these are what we call as the most common type of tardive dyskinesia movements are the oral buccolingual movements. These are very common presentation of tardive dyskinesia. The social isolation part, it is challenging because think about it, we are giving, we are treating the patient for a condition that is distressing. And the symptoms or these movements symptoms that he is having is a side effect of the medication. It is always a challenge especially when the treatment has been working or the patient has been stable. But the good thing is until about 3 years ago, we did not have any medication that was specifically, that we could use or approved by the FDA [Food and Drug Administration] to treat tardive dyskinesia. Now that we have the medication, I think the treatment decisions are slightly a bit better than before. Because before it is always about, what do we do? The patient is stable. It has always been a balance between a choice, a treatment choice between the benefit versus the risk and the adverse effect. How much is it affecting the patient? Now we can treat it with, if the patient has been stable, we do not need to stop the medication. If the patient and the family is comfortable with the treatment, we do have a treatment choice that could help the patient. And the level of evidence is strong that VMAT2 inhibitors do work well for tardive dyskinesia symptoms.
Transcript edited for clarity.
Newsletter
Receive trusted psychiatric news, expert analysis, and clinical insights — subscribe today to support your practice and your patients.