Treating Tardive Dyskinesia With a VMAT2 Inhibitor
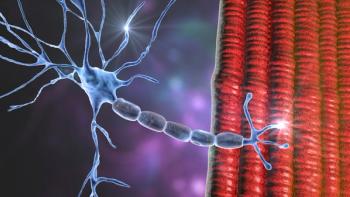
In this custom video series, recommendations regarding patient selection and use of VMAT2 inhibitors in patients with tardive dyskinesia based on current clinical guidelines and real-world practice are shared.
Episodes in this series

Leslie L. Citrome, MD, MPH: There are some additional points I’d like to talk about before we finish. Who should get treated? Should it be anyone with any movement? Should it be only those with severe movements? I know we touched on it earlier, but I’d like to end up talking about how we approach the TD [tardive dyskinesia] management. What would be the urgency to treat? Let’s reinforce those points.
Rose Mary Xavier, PhD, MS, RN, PMHNP-BC: The guidance should come from how it’s affecting the patient. It doesn’t matter if it’s mild vs severe. TD is persistent. It can range in severity from mild to severe, but it does affect the patient’s quality of life and it has a huge psychological impact on the patient. Sometimes clinicians aren’t aligned with what the patients need specifically when it comes to an iatrogenic symptom like an adverse effect of the treatment per se. For example, women like to put makeup on, and it’s very hard if you have even a mild tremor to put on lipstick or eyeliners. How often do our clinicians ask about their self-care and how they feel about themselves and the quality of life they have? It depends on the patient. This conversation is an absolute must. We should be talking to our patients. The blanket rule, visual assessment, every time: If you see TD, go ahead and do the formal structured assessments and talk to the patient, talk to the family members, ask about how it’s affecting their life. We’re treating patients so we can make their life better, and if we’re adding to it, and if that’s not a measure of evaluation, we’re losing and not doing a proper job.
Leslie L. Citrome, MD, MPH: Thank you for that. It’s not just a matter of assessing the movements and measuring how bad they are on the aims. It’s also assessing the impact these movements have on the person whom you’re working with to recover. Part of the recovery journey is to manage everything, to make their lives better for them. If they have movements, it’s going to be stigmatizing. Other people will notice them, even if the patients themselves aren’t completely aware, little incremental changes can go a long way.
I often find it helpful to mention the American Psychiatric Association guidelines for the treatment of schizophrenia, which were recently revised. It’s available for free online. They talk about the management of drug-induced motor adverse effects. They talk about TD in a way they never had before. The guidelines recommend the use of VMAT2 inhibitors, and that recommendation was unanimous based on the evidence, which was considered very convincing and gave it their highest rating. They suggested that people being treated with antipsychotics should be evaluated periodically. In fact, as often as feasible for abnormal motor adverse effects and formally on a scheduled basis. They also recommend, in the presence of moderate to severe TD, that they be treated with a VMAT2 inhibitor. They also mentioned that those with mild TD can be treated. It depends on the patient’s degree of awareness and also the degree of functional impairments that they may be experiencing.
The door is open to the treatment of tardive dyskinesia, from mild on up, for people who need it, and the treatment guidelines certainly encourage us to do so. Now we have treatments available that work quite well.
Transcript edited for clarity.
Newsletter
Receive trusted psychiatric news, expert analysis, and clinical insights — subscribe today to support your practice and your patients.