Also in This Special Report
Exploring the Connections Between Mental Health and Our Environment
Elizabeth Haase, MD
Connections Between Food Additives and Mental Health Disorders
Ruo-Gu Xiong; Jiahui Li; and Hua-Bin Li, PhD
Publication
Article
Psychiatric Times
Author(s):
Climate change is a global public health crisis.
Flowstudio/AdobeStock

SPECIAL REPORT: PSYCHIATRY & THE ENVIRONMENT
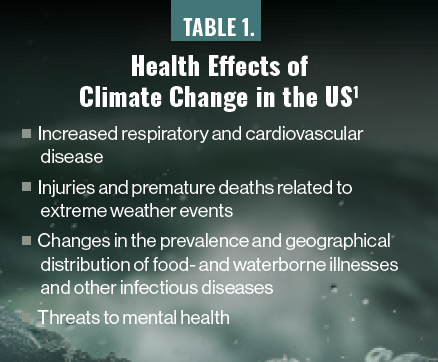
Climate change presents a global public emergency with drastic impact on human physical and mental health. As most research has been happening in Western countries, there is a lack of information from developing countries. The health effects of these disruptions in the US, according to the CDC, are listed in Table 1.1 Climate change is considered a destructive reality with severe consequences for the future. The World Health Organization estimates an increase of 250,000 excess deaths per year between 2030 and 2050 due to the “well-understood impacts of climate change.”2
Table 1. Health Effects of Climate Change in the US1
The connection between climate change and mental health is still underresearched, primarily because of the heterogeneity of studies to measure the impact of climate change on mental health. Explanatory models have proposed direct and indirect effects of climate change on mental health.3 Direct effects include stress- and trauma-related outcomes of acute events such as floods or hurricanes, whereas indirect effects describe more insidious mental health changes related to physical health, such as increased ambient temperature; increased pollen, dust, or pollution; and community-level impacts from economic damages, scarce natural resources, displacement, or migration due to loss of habitable land.4
The impacts on mental health can vary from distress to clinical disorders such as depression, anxiety, posttraumatic stress disorder (PTSD), insomnia, and suicidal thoughts.5 For example, a study by Thompson et al6 showed that increased temperature and temperature variability could be associated with increased cases of suicide and suicidal behavior, hospital attendance or admission for mental illness, and poor community health and well-being. Individuals with preexisting mental health conditions such as dementia are more vulnerable to the impacts of heat waves and are at higher risk for hospitalization and death during them.7
Using comprehensive data from multiple decades for both the US and Mexico, another study found that suicide rates rise 0.7% in US counties and 2.1% in Mexican municipalities for a 1 °C increase in monthly average temperature.8 In addition, high temperatures and low precipitation increase the chances of drought, which can last decades.9
There are 2 major pathways through which drought has been empirically linked to adverse mental health outcomes. The first involves the economic effects of drought, which can adversely impact individual and community economic activities, particularly livelihoods influenced by weather conditions and water access. The second is the migration pathway, which brings social and geographical isolation and increases the risk for depression and anxiety.10
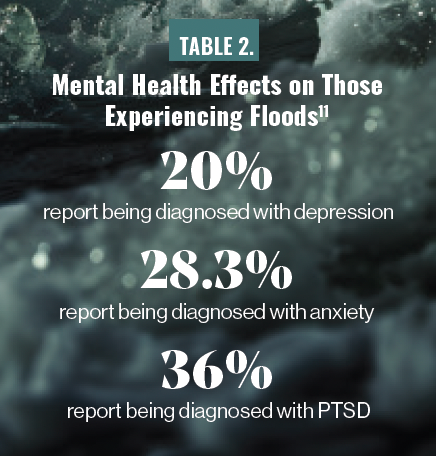
Another global climate impact that requires attention is flooding. As described by Cianconi et al,11 flooding is studied globally in many nations and is known to cause grief, displacement, and psychological distress due to loss of lives and possessions. This same study also reported that 20% of those experiencing floods had been diagnosed with depression, 28.3% with anxiety, and 36% with PTSD (Table 2).11 There was reported increased use of tobacco and alcohol in Australia but the same was not found in the US and Canada.12 Overall psychological health-related quality of life was significantly worse in affected areas compared with nonaffected areas.12
Table 2. Mental Health Effects on Those Experiencing Floods11
Wildfires pose an escalating public health hazard, as they generate an immense volume of smoke-related pollution, including carbon monoxide, nitrous oxide, ozone, aromatic hydrocarbons, and particulate matter less than 2.5 μm in diameter.13 Studies have suggested that higher rates of PTSD in the pediatric and adult populations are ascribed to witnessing homes burning, experiencing fear for one’s life or the lives of loved ones, losing loved ones, enduring substantial property damage, or perceiving a lack of support from family and friends.14 These symptoms have been shown to persist from 3 months up to 10 years post wildfire.15 There are also higher rates of depression, alcohol and tobacco use, and insomnia in populations exposed to wildfires.16,17
Climate change is a social determinant of mental health. There is a disproportionate impact on vulnerable populations such as inhabitants of low-income countries like India, China, and Brazil; refugees; migrants; and individuals experiencing homelessness. Women, older adults, children, and members of ethnic minority populations are also more at risk. Climate-related anxiety has also been given a new term—eco-anxiety, defined by the American Psychological Association as “the chronic fear of environmental cataclysm that comes from observing the seemingly irrevocable impact of climate change and the associated concern for one’s future and that of next generations.”18
Intervention Strategies
Exploring the Connections Between Mental Health and Our Environment
Elizabeth Haase, MD
Connections Between Food Additives and Mental Health Disorders
Ruo-Gu Xiong; Jiahui Li; and Hua-Bin Li, PhD
Advocacy by mental health clinicians is important to help with awareness of climate change and its impact on mental health. Although it is crucial to work on prevention, as climate change becomes more prevalent it is important for mental health clinicians to be aware of its impact on mental health. Clinicians working in mental health and primary care should be able to assess and manage the impact of climate change on mental health.
Most recent literature about effective interventions addresses community involvement. Health promotion, education, and early intervention have been found to be effective in helping with resiliency in Australia.19 Social cohesion among families and communities has been found to be helpful. For mental health clinicians and primary care providers, medical education on climate change and mental health has been useful in helping patients in Canada.20
Research in the United Kingdom shows that households with proenvironmental behavior are associated with positive mental health outcomes, whereas individual-level proenvironmental behaviors have a more mixed impact on mental health.21 Considerable evidence suggests that involving local communities, utilizing local knowledge, and working in an interdisciplinary team (with other health care providers like psychologists, counselors, and first responders) can be helpful in mitigating mental health impacts.
For long-lasting climate-related events, it is important to focus on relocation, education, engagement, and positive psychological outcomes. For patients who have “eco-anxiety,” it is important to acknowledge that it can be paralyzing and can lead to helplessness.22,23 Working in collaboration with other stakeholders like climate scientists and policymakers can also help with advocacy, outreach, and implementation of preventive and intervention programs.
Climate Change and Mental Health Curriculum
There is a lack of training in climate change and mental health for medical students and residents. Psychiatrists also need additional education about the relationship between climate change and mental health. Four out of 10 students graduating from US medical schools between 2009 and 2013 reported receiving inadequate education on climate change.24 Globally, a survey conducted in 112 countries that included information from 2817 medical schools reported that only 15% of schools had a curriculum on climate change and health.25
There is a need for specific training and curricula within medical school and residency programs about climate change and more CME activities discussing mental health and climate change. Although many medical schools and residency training programs are coming up with curricula, they face barriers such as insufficient resources, lack of experts, climate-related anxiety, and difficulty identifying ways to evaluate.26 Perhaps creating interdisciplinary educational programs across medicine, psychiatry, psychology, and social science will help with pulling resources and knowledge together.
Concluding Thoughts
Climate change is a global public health crisis. There is increasing evidence about how climate change relates to mental health. It has an impact not just on the mental health of individuals who are experiencing climate change but also on those who have not experienced climate-related disasters. Clinicians need to be aware of this impact and of strategies for prevention and intervention. Supporting vulnerable populations, clinician education, actions to address climate change, and investment in more research and treatments will help take this a long way.
Dr Marwaha is psychiatry residency training director, vice chair of education and faculty development, interim child and adolescent psychiatry division director, and associate professor at Case Western Reserve University, MetroHealth System, in Cleveland, Ohio. He is also president of the North East Ohio Society of Child and Adolescent Psychiatry and president of the Caucus of International Medical Graduates, American Psychiatric Association.
Dr Malhi is program director of the psychiatry residency program at ChristianaCare and medical director of the Child and Adolescent Psychiatry Clinic and Multidisciplinary Autism Program at ChristianaCare, Delaware.
References
1. Climate effects on health. CDC. Updated April 25, 2022. Accessed March 8, 2024. https://www.cdc.gov/climateandhealth/effects/default.htm
2. Watts G. Scientists welcome new global climate change pact. Lancet. 2015;386(10012):2461-2462.
3. Berry HL, Bowen K, Kjellstrom T. Climate change and mental health: a causal pathways framework. Int J Public Health. 2010;55(2):123-132.
4. Hwong AR, Wang M, Khan H, et al. Climate change and mental health research methods, gaps, and priorities: a scoping review. Lancet Planet Health. 2022;6(3):e281-e291.
5. Ursano RJ, Morganstein JC, Cooper R. Resource Document on Mental Health and Climate Change. American Psychiatric Association. Accessed March 8, 2024. https://www.psychiatry.org/getattachment/b7fb9e58-86f7-4b54-bd32-59fb50f32d9c/Resource-Document-2017-Mental-Health-Climate-Change.pdf
6. Thompson R, Lawrance EL, Roberts LF, et al. Ambient temperature and mental health: a systematic review and meta-analysis [published correction appears in Lancet Planet Health. 2023 Sep;7(9):e735]. Lancet Planet Health. 2023;7(7):e580-e589.
7. Gong J, Part C, Hajat S. Current and future burdens of heat-related dementia hospital admissions in England. Environ Int. 2022;159:107027.
8. Burke M, González F, Baylis P, et al. Higher temperatures increase suicide rates in the United States and Mexico. Nature Clim Change. 2018;8:723-729.
9. Demetillo MAG, Anderson JF, Geddes JA, et al. Observing severe drought influences on ozone air pollution in California. Environ Sci Technol. 2019;53(9):4695-4706.
10. Vins H, Bell J, Saha S, Hess JJ. The mental health outcomes of drought: a systematic review and causal process diagram. Int J Environ Res Public Health. 2015;12(10):13251-13275.
11. Cianconi P, Betrò S, Janiri L. The impact of climate change on mental health: a systematic descriptive review. Front Psychiatry. 2020;11:74.
12. Fernandez A, Black J, Jones M, et al. Flooding and mental health: a systematic mapping review. PLoS One. 2015;10(4):e0119929.
13. Why wildfire smoke is a health concern. US Environmental Protection Agency. Updated October 13, 2023. Accessed March 8, 2024. https://www.epa.gov/wildfire-smoke-course/why-wildfire-smoke-health-concern
14. Malhi NK, Marwaha R. Running wild: the impact of wildfires on mental health. Psychiatric Times. October 12, 2023. Accessed March 8, 2024. https://www.psychiatrictimes.com/view/running-wild-the-impact-of-wildfires-on-mental-health
15. To P, Eboreime E, Agyapong VIO. The impact of wildfires on mental health: a scoping review. Behav Sci (Basel). 2021;11(9):126.
16. Brown MRG, Agyapong V, Greenshaw AJ, et al. Significant PTSD and other mental health effects present 18 months after the Fort McMurray wildfire: findings from 3,070 grades 7-12 students. Front Psychiatry. 2019;10:623.
17. Isaac F, Toukhsati SR, Di Benedetto M, Kennedy GA. A systematic review of the impact of wildfires on sleep disturbances. Int J Environ Res Public Health. 2021;18(19):10152.
18. Whitmore-Williams SC, Manning C, Krygsman K, Speiser M. Mental Health and Our Changing Climate: Impacts, Implications, and Guidance. American Psychological Association; March 2017. Accessed March 8, 2024. https://www.apa.org/news/press/releases/2017/03/mental-health-climate.pdf
19. Hart CR, Berry HL, Tonna AM. Improving the mental health of rural New South Wales communities facing drought and other adversities. Aust J Rural Health. 2011;19(5):231-238.
20. Valois P, Blouin P, Ouellet C, et al. The health impacts of climate change: a continuing medical education needs assessment framework. J Contin Educ Health Prof. 2016;36(3):218-225.
21. Netuveli G, Watts P. Pro-environmental behaviours and attitudes are associated with health, wellbeing and life satisfaction in multiple occupancy households in the UK Household Longitudinal Study. Popul Environ. 2020;41:347-371.
22. Pinsky E, Guerrero APS, Livingston R. Our house is on fire: child and adolescent psychiatrists in the era of the climate crisis. J Am Acad Child Adolesc Psychiatry. 2020;59(5):580-582.
23. Hickman C, Marks E, Pihkala P, et al. Climate anxiety in children and young people and their beliefs about government responses to climate change: a global survey. Lancet Planet Health. 2021;5(12):e863-e873.
24. Finkel ML. A call for action: integrating climate change into the medical school curriculum. Perspect Med Educ. 2019;8(5):265-266.
25. Omrani OE, Dafallah A, Paniello Castillo B, et al. Envisioning planetary health in every medical curriculum: an international medical student organization’s perspective. Med Teach. 2020;42(10):1107-1111.
26. Seritan AL, Coverdale J, Brenner AM. Climate change and mental health curricula: addressing barriers to teaching. Acad Psychiatry. 2022;46(5):551-555.
Receive trusted psychiatric news, expert analysis, and clinical insights — subscribe today to support your practice and your patients.