
Dance/movement therapy has proven to be effective in treating children with trauma, making dance something that can change the way a child develops psychologically.

Dance/movement therapy has proven to be effective in treating children with trauma, making dance something that can change the way a child develops psychologically.

"I refuse to see sexual violence as a 'women’s issue.' It is a human issue and should be addressed as one."

How can we prevent retraumatization of vulnerable individuals and enable them to seek redress?
In this CME article, learn more about the best practices for engaging patients in the informed consent process for psychedelic treatment and psychedelic-assisted psychotherapy.

The law presumes that individuals are rational. But what about when the patient has neuropsychiatric impairments that hinder judgement?

We seek to reduce vaccine side effects—but what about the social media-compounded fears of anti-COVID vaccination?

One doctor shares how family history and art have inspired him.

The emergence of epigenetic models has generated a surge of optimism, opening new possibilities for psychiatric intervention.

In this CME, learn how to design interventions to promote resilience, study their relative effectiveness, and implement them accordingly.
What 6 things are important to keep telemedicine practice running smoothly?

When meeting patients online, mental-health practitioners must confront a host of issues.

Schools need to be at the heart of our response to the COVID-19 mental health crisis.

Mental health providers who battle a pandemic may find that it unsettles their deepest sense of self.

The cure should not be worse than the disease; so must we be cautious about our response to COVID-19. More in this video with Harold J. Bursztajn, MD.
In a time of panic, despair, and demoralization, art continues to inspire the author's reflections as it has over the last 40 years. Here, he shares some images that he finds inspirational and helpful. Even in winter there is hope.

Local, state, and federal officials are rushing to implement massively life-altering measures in the current pandemic even as we enter a situation that is still poorly understood.
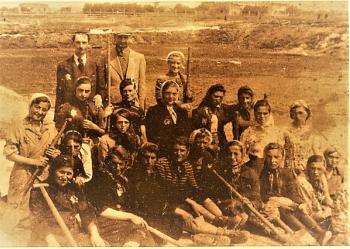
For an inspiring model of communal hope and resilience under a dire threat to survival over COVID-19 fears, the author turns to the Fekalists, the prisoners condemned to be sanitation workers in the Lodz ghetto in Nazi-occupied Poland, his parents among them.
This article explores why Enduring Personality Change After Catastrophic Experience (EPCACE) is a clinically useful diagnosis.
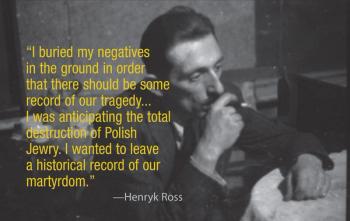
As I’ve seen in my parents’ remarkable journey from the doomed Jewish ghetto in Lodz, Poland, and in my psychiatry practice, photographs have immense power to heal.
The authors explore possible reasons why young people in the West leave their families, friends, and home culture to join terrorist organizations.

The grief that the Shoah brought to its victims would make its reappearance even at happy times long afterwards.

I was 9 years old in December 1959 when I left and 60 in July 2011 when I returned to Lodz, Poland. My return-a journey through time as well as space-was a continuation of a trip from my home in Cambridge, Massachusetts, where I teach and practice clinical and forensic psychiatry, to Berlin, where I gave a number of presentations at a conference of the International Academy of Law and Mental Health (IALMH).

When working with patients who are at high risk for relapse or misuse of prescription medications, careful documentation of the informed consent process is a helpful risk management tool.

Questions have also been raised about the extent of industry influence on the American Psychiatric Association’s diagnostic and treatment guidelines-namely, its DSM and Clinical Practice Guidelines.

In response to increasing public distrust and congressional concerns regarding pharmaceutical company influence on medical research and education, professional organizations have taken steps to phase out or regulate industry-sponsored educational support. A related problem is industry funding of philanthropic organizations, such as patient advocacy groups. Thus, when the office of Sen Charles Grassley (R-Iowa) recently reported that the National Alliance for the Mentally Ill received substantial pharmaceutical funding, there was concern among the membership’s psychiatric patients and their families.

Following trends in medicine, psychiatry is faced with limited resources and third-party administration of resource allocation. This has affected psychiatric practice in many ways and altered the doc-tor-patient relationship. Trends toward resource-sensitive, third-party–related psychiatric practice may be accelerated by the current social concerns regarding the economy. Thus, an awareness of social context and the growing recognition that autonomy-enhancing alternatives to paternalistic care are fundamental to improve both the effectiveness and accessibility of care in limited-resource environments are each becoming vital for an informed clinical and risk-management practice perspective.1

Physicians are often conflicted regarding prescription medications for pain, especially pain complicated by insomnia and anxiety. Concerns that patients may become addicted to medications, exacerbated by limited time available to get to know patients, can lead to underprescribing of needed medications, patient suffering, and needless surgery. At the other extreme, pressure to alleviate patients' distress can lead to overprescribing, needless side effects, and even addiction.

Recent discoveries in neuroscience have ramifications for all aspects of clinical and forensic practice, including diagnosis, treatment, and testimony in civil and criminal justice cases.

Published: December 21st 2020 | Updated:

Published: October 1st 2020 | Updated:

Published: August 24th 2023 | Updated:

Published: March 12th 2025 | Updated:

Published: June 14th 2021 | Updated:
Published: September 10th 2015 | Updated: