Publication
Article
Psychiatric Times
Bioethical Challenges for Psychiatrists: Determination of Decisional Capacity
Author(s):
The authors parse myths and facts about decisional capacity, with the goal of preserving patients' dignity and autonomy and helping you mediate conflicts, meet bioethical challenges, and provide compassionate resolutions.
Table 1 – Patient-related myths and facts[16]
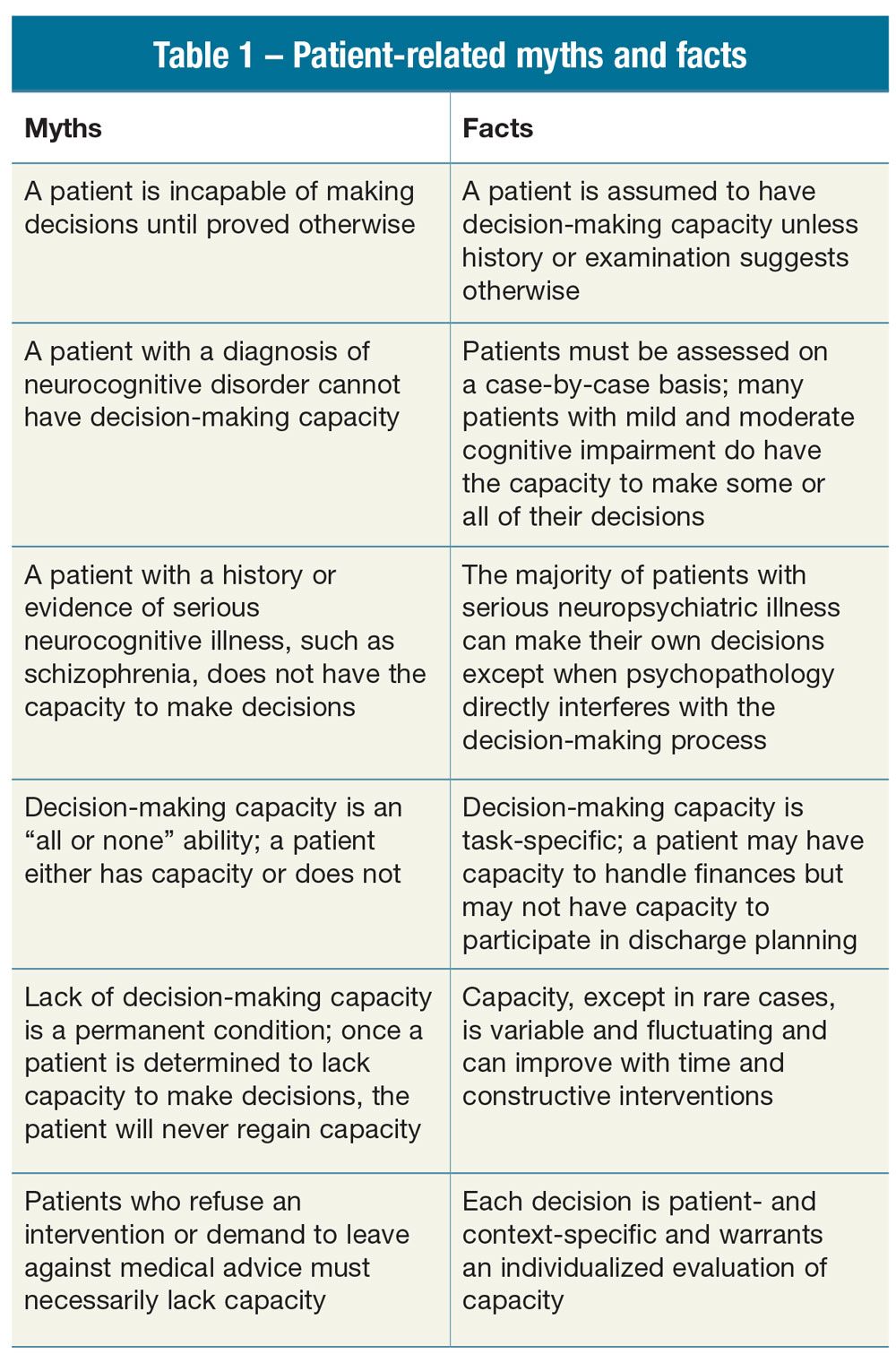
Table 2 – Examples of psychopathology that interferes with decisions
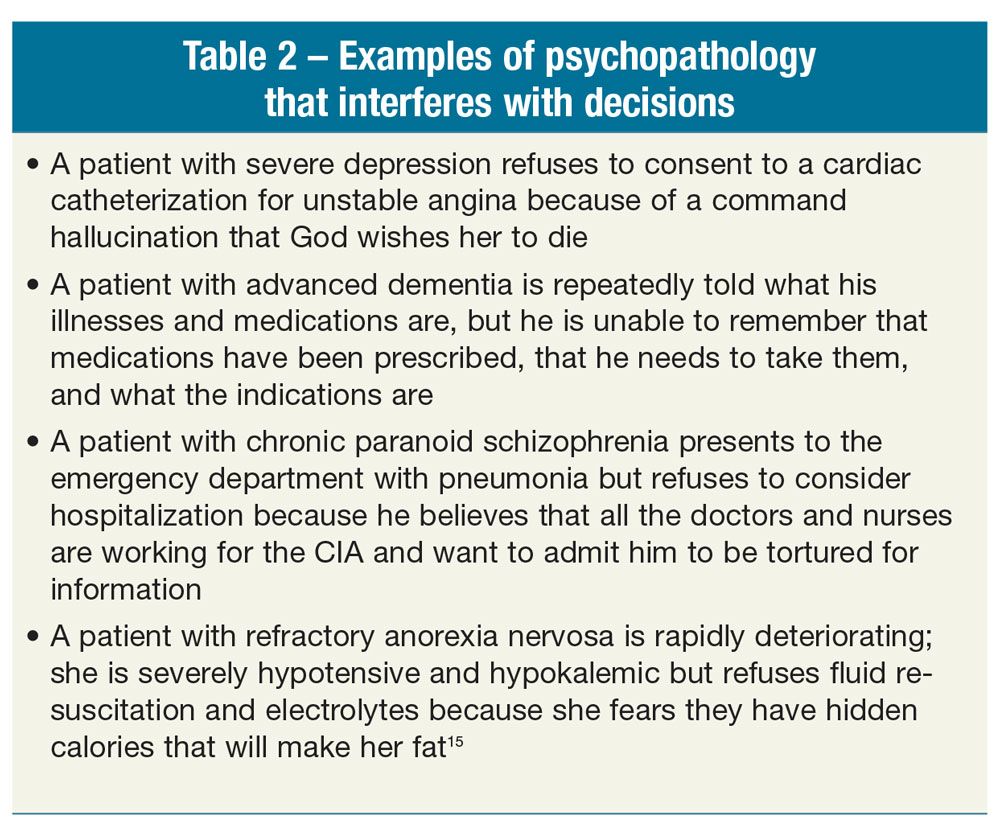
Table 3 – Common capacity questions submitted to psychosomatic medicine services
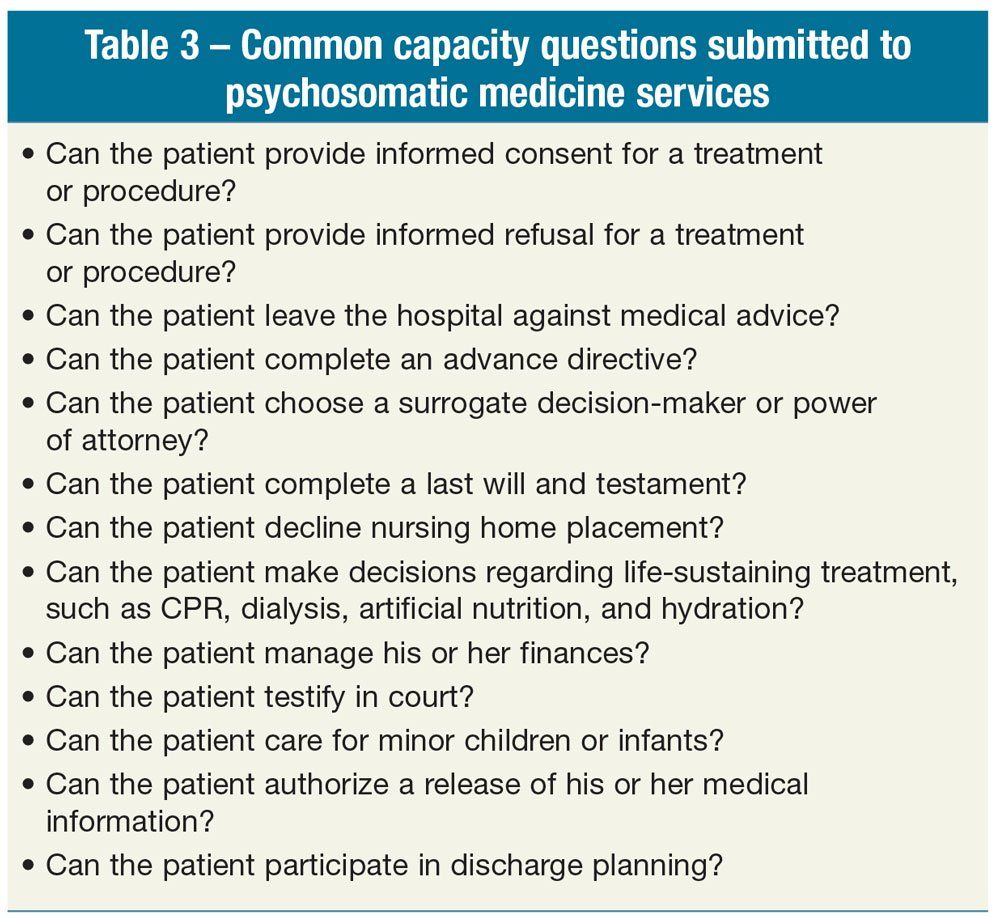
Table 4 – Practitioner-related myths and facts[16]
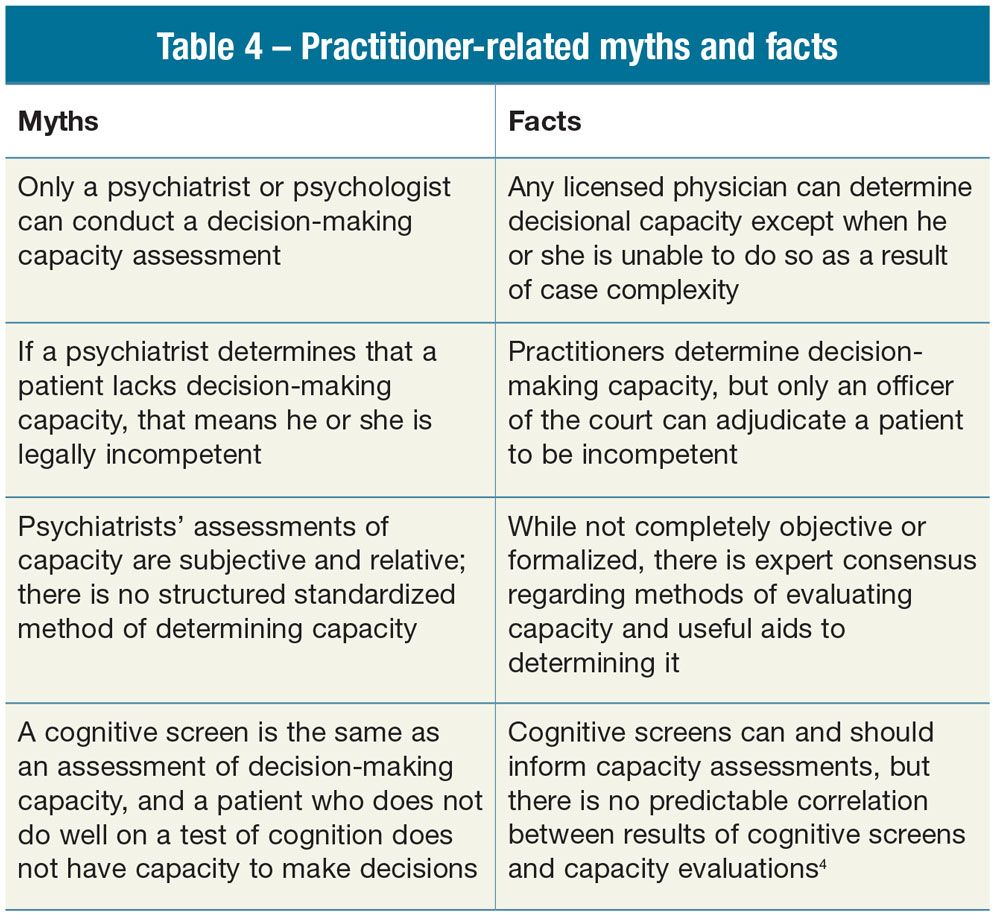
Table 5 – Components of decision-making capacity
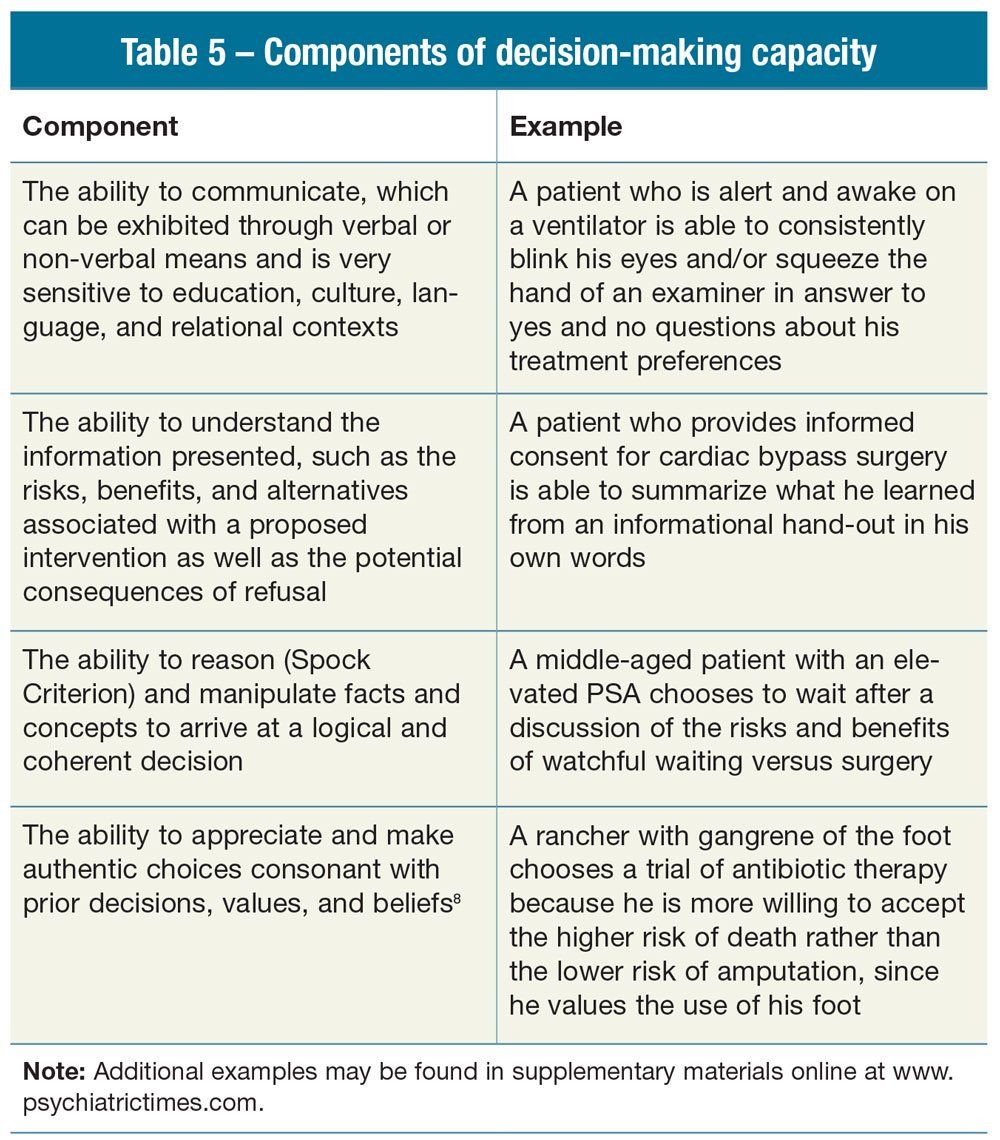
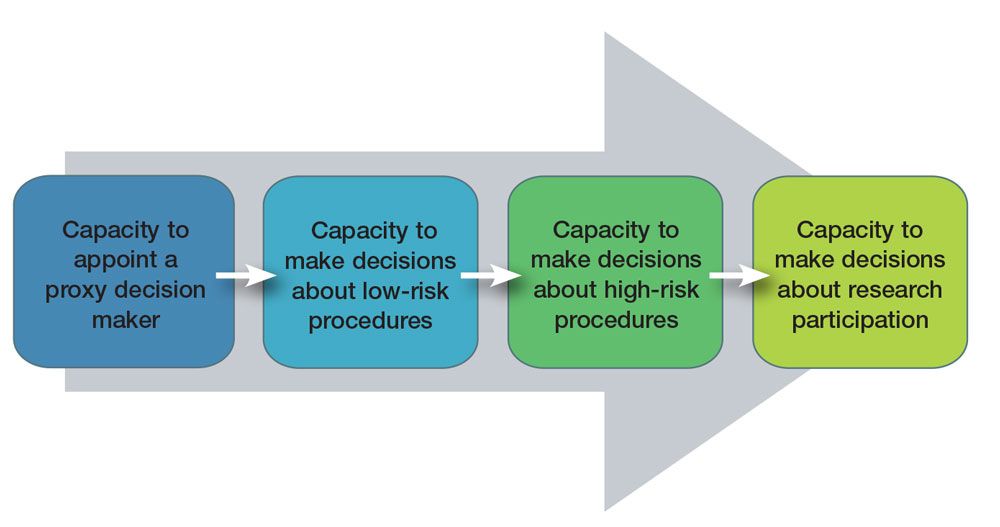
Figure. Increasing levels of decisional capacity
Evaluations of decisional capacity are among the most common-and the most complex-psychiatric consultations. Determination of decisional capacity is fraught with myths that may mislead all physicians. These misunderstandings present clinical pitfalls that can result in serious medical, ethical, legal, and psychosocial challenges. Conversely, the ability to conduct a decision-making capacity assessment with knowledge, skill, empathy, and wisdom is a duty and service of high ethical value and significance. Decisional capacity assessments that psychosomatic medicine psychiatrists perform every day help protect vulnerable individuals from neglect and exploitation, preserve autonomy and self-determination, and help other clinicians and administrators solve complex bioethical and biomedical dilemmas.
These evaluations provide a forum for the entire health care community and its stakeholders to engage in thoughtful deliberations that inform policy development that upholds the highest ethical values of our profession and society regarding medical care and research.
This article will focus on capacity to participate in medical decisions rather than research, but there is considerable overlap in the principles and procedures presented.
Facts and myths about decision-making capacity
One of the most important reasons to tease apart the facts from the myths is that so many of the individuals for whom capacity assessments are requested have psychiatric disorders, such as schizophrenia and dementia (Table 1). The majority of patients with schizophrenia and most patients with mild to moderate dementia are-with psychiatric care, assistance, patience, kindness, and time-able to make many basic medical and dispositional decisions.1
Many clinicians, including psychiatrists, may confuse and conflate commitment and capacity, not recognizing that many patients who are committed retain the ability to participate in treatment decisions.
Findings from a recent study of over 2500 patients indicate that, contrary to the hypothesis of the research, it was not psychosis that led to incapacity but rather cognitive impairment and substance use.2 The exception is when the psychopathology directly interferes with the patient’s decision-making process as in the frequently encountered case examples in Table 2.
The presumption that patients with psychopathology do not have decisional capacity is often grounded in an even more profound misunderstanding of decision-making capacity as monolithic: that decisional incapacity in one area, such as finances, precludes capacity in all areas. Most of us are able to make better decisions in some areas of our lives than in others. Similarly, it is often assumed that capacity is static, when it is really a dynamic, granular ability that is better at some times and worse at others.
Delirium is among the most frequently encountered, yet often unrecognized, conditions that impair the capacity of patients to make decisions in the settings of emergency departments as well as medical, surgical, and intensive care units.3 Because of the intrinsically fluctuating nature of delirium, which typically worsens toward evening, and our obligation to offer the patient an optimal opportunity to perform well on the assessment, it is often best to conduct capacity evaluations in the morning-especially for patients with or at risk for delirium.
Yet this variability is also a positive: it means that we can enhance a patient’s ability through basic interventions we know well as psychiatrists, such as normalizing the sleep-wake cycle; treating anxiety, depression, and psychosis; and providing supportive psychotherapy. Both pharmacological and psychological treatments as well as a variety of cultural adjustments, such as having a trained interpreter and educational modalities (eg, audiovisuals, social supports involving family members), have been shown to improve the ability of patients with physical and psychiatric illnesses to optimize their decisional capacity. Ethically, it is our obligation to try these interventions so that we give the patient the “best chance” to do as well as possible and to assess the patient at the point of his or her highest capacity.
An essential aspect of this “best chance” is that the psychiatrist must define the object of the capacity request. The first thing we teach psychiatric residents who respond to a consultation request for capacity determination is to discuss with the requesting clinician, “Just exactly what is the question?” This helps to begin a dialogue and to elicit the latent as well as the manifest content of the consultation question. A study examined 100 consecutive consultations for capacity evaluations submitted to a psychosomatic medicine service at an academic medical center. The results of this study showed that approximately the same number of consultations were received for the capacity to consent to a treatment or procedure, the capacity to refuse a treatment or procedure, the capacity to leave the hospital against medical advice, and the capacity to accept or reject a discharge plan (Table 3).4
Competence versus capacity
The importance of patient self-determination requires that, at the outset, we recognize the legal limits of medical capacity assessments. Only a judge or other officer of the court can make the legal determination of competence. Although our capacity assessments often inform the court’s decision, medical assessments of incapacity are not formal legal adjudications that patients are incompetent with all the attendant limitations on their rights and responsibilities as citizens. Although some experts believe this distinction is purely semantic, the 2 terms functionally refer to quite distinct but related processes.
This is an especially salient distinction when applied to patients with psychiatric disorders who have been involuntarily committed. Many clinicians, including psychiatrists, may confuse and conflate commitment and capacity, not recognizing that many patients who are committed retain the ability to participate in treatment decisions and provide informed consent (Table 4). Conversely, there is an inherent assumption that when a patient refuses a recommended hospitalization, test, or procedure or suggested medical treatment, he or she “must be mentally ill.” Similar to innocence in our system of criminal justice, in Anglo-American bioethics, the patient should be presumed capacitated unless it is clear that the refusal is based on a psychiatric disorder that is interfering directly with the decision-making process. Persons with neuropsychiatric illness have the same rights as all patients and can refuse or consent to medical care.5
Determination of decisional capacity: who and how?
While law and policy endow any physician with the requisite training and scope of practice to perform a capacity evaluation, in reality, when non-psychiatric physicians are struggling with the evaluation or are confronted with a particularly complicated patient, they often turn to psychosomatic physicians to conduct the assessment. A study that compared the capacity of medical inpatients to make major decisions using the Mini-Mental State Examination (MMSE), clinical impression, and expert evaluation showed that the MMSE and clinical impression were often inaccurate predictors of decision-making.6 However, this does not mean that there is no structured or standardized approach for performing capacity assessments. A widely accepted and utilized method for analysis of decisional capacity is Appelbaum’s7 approach of using 4 key components (Table 5).
Communication and understanding can be conceptualized as the lower order of abilities necessary to make the most basic decisions, such as choosing a surrogate, while rationality and appreciation are higher-order abilities needed for complex decisions, such as selecting surgery, chemotherapy, or radiation for cancer. Using the MacArthur Assessment Tool, Owen and colleagues8 found that patients who scored low on the understanding component were not likely to be capacitated. Appreciation was a better test of capacity in psychiatric patients, while reasoning was superior in those with systemic medical disorders. The correlation of brain imaging with specific capacity impairments is in its infancy but is a promising future direction for capacity research.9
In assisting patients and clinicians to determine whether a patient has the capacity to make difficult and life-changing decisions, psychosomatic medicine physicians are fortunate to have access to several useful decision aids. The MacArthur Competence Assessment Tools for Clinical Research and Treatment is the most evidence-based tool, and the Aid to Capacity Evaluation (ACE) is among the most clinically useful.10,11 These instruments can provide results that can also support psychosomatic medicine psychiatrists in the presentation of their findings to other clinicians and family members and document the results of an evaluation in a formal report suitable for submission to social service agencies or courts.
Also see:
Of Blood and Truth
One of the most significant pitfalls to avoid when using any structured instrument is to realize that it cannot supplant-only supplement-the clinical evaluation. Research suggests that medical patients who score on the low end of the range on cognitive instruments are more likely to lack decision-making capacity; similarly, those with near-normal scores are probably able to make decisions. In the middle range, however, there is no exact or predictable correlation.12
The decisional capacity gradient
It is precisely in the most complex of capacity evaluations where relevant clinical context is crucial and where a clinical “gradient” decisional capacity model can be highly beneficial in formulating the evaluation. On this gradient, capacity is conceived as “dimensional,” in that different decisions require different levels of sophistication (Figure). It is important to recall that many otherwise cognitively impaired patients may at least name a surrogate decision maker.
As such, assessment for the capacity to name a surrogate (can the patient understand the role of a surrogate, when the surrogate would be used, and that the surrogate may not make the decision the patient “would have wanted”) is often a practical matter, even if the patient cannot demonstrate decisional capacity for the medical or surgical intervention at hand. While some have criticized sliding-scale types of models, Appelbaum7 points out the considerable policy and practical advantages of the approach.13
The gradient of capacity should remind the capacity evaluator that even patients who perform poorly on cognitive screens may have intact functional capacity and are able to care for themselves in the community through routine and a network of friends and family; or a patient with progressive cognitive impairment may have “good old-fashioned common sense” and recognize, for example, that he is unsafe at home and agree to assisted living. In these decisions, balancing respect for patient autonomy and the duty to keep the patient safe are the paramount ethical values in conflict.
Evaluators must be cautious to avoid too quickly substituting their preferences as a substituted judgment. Refusal of care, including psychiatric treatment, accentuates this challenge.
In consultations to determine the patient’s future decisional capacity for independent living and self-care (ie, “dispositional capacity”), as opposed to a decision about a specific medical intervention-where the Appelbaum and Grisso framework is most clearly applicable-additional consultation with an occupational therapist for a Kohlman Evaluation of Living Skills and similar in vivo dynamic assessment of self-care skills may greatly add to the psychiatrist’s assessment.
Ethical challenges
Ethical challenges are intensified in marginalized and underserved populations, such as individuals who are undomiciled or marginally housed, undocumented immigrants, the elderly, and persons with addiction or other psychiatric disorders-all of whom are vulnerable to exploitation and victimization. Ironically, although we recognize the fragile position of the economically disadvantaged and incapacitated, the wealthy can also be vulnerable and victimized. Take, for example, the widely publicized case of Brooke Astor whose son stole and sold artwork and other valuables worth millions from his mother, including works of art that she personally treasured.
Emerging research on the challenges of determining capacity in persons who are undomiciled is illustrative of the difficulties in evaluating decision-making in marginalized groups. When caring for undomiciled individuals, clinicians may struggle with feelings of anger-directed at “the system” or the undomiciled individual-lack of empathy, disgust, and even futility.14 These emotional responses can impair objective assessment of patient needs, decisional capacity, and reaction to behaviors. There may be an excessive reluctance to discharge undomiciled patients, even with resolution of acute medical needs. Alternatively, there may be a risk of refusing care or of faster than indicated discharge as a consequence of negative countertransference to the undomiciled individual.
Evaluators must be cautious to avoid too quickly substituting their preferences as a substituted judgment. Refusal of care, including psychiatric treatment, accentuates this challenge. Legal precedents have supported the right of homeless psychotic individuals to refuse care. When considering capacity in a homeless individual, the same general standards need to be applied, while keeping in mind some of the potential complicating factors:
• Higher symptom burden
• Distrust of medical profession based on prior encounters
• Higher potential for medical consequences of refusing care
• Risk of alienation from future care with forced treatment
Conclusions
There is no one-size-fits-all in decisional capacity. Every assessment is determined on a case-by-case basis. Understanding the myths and facts about decisional capacity allows patients to preserve dignity and autonomy and helps clinicians mediate conflicts, meet the bioethical challenges of determination of decisional capacity, and provide compassionate resolutions for both patients and their caregivers.
Acknowledgment-The authors acknowledge Christina Wichman, DO, FAPM, and Catherine C. Crone, MD, of the Academy of Psychosomatic Medicine (APM) for helping bring this article to fruition. The APM is the professional home for psychiatrists providing collaborative care bridging physical and mental health. Over 1200 members offer psychiatric treatment in general medical hospitals, primary care, and outpatient medical settings for patients with comorbid medical conditions.
Disclosures:
Dr. Geppert is Professor of Psychiatry and Director of Ethics Education, University of New Mexico School of Medicine; and Chief, Consultation Psychiatry and Ethics, New Mexico VA Health Care System, Albuquerque, NM. Dr. Cohen is Clinical Professor of Psychiatry, Icahn School of Medicine at Mount Sinai, New York. Dr. Bourgeois is Clinical Professor and Vice Chair of Clinical Affairs, department of psychiatry, Langley Porter Psychiatric Institute, University of California, San Francisco. Dr. Peterson is Associate Professor in Psychiatry, University of Wisconsin School of Medicine and Public Health and Director of Hospital Psychiatric Services, University Hospital, Madison, WI. The authors report no conflicts of interest concerning the subject matter of this article.
References:
1. Dunn LB, Gordon NE. Improving informed consent and enhancing recruitment for research by understanding economic behavior. JAMA. 2005;293:609-612.
2. Boettger S, Bergman M, Jenewein J, Boettger S. Assessment of decisional capacity: prevalence of medical illness and psychiatric comorbidities. Palliat Support Care. 2015;13:1275-1281.
3. Ganzini L, Mansoor D, Socherman R, Duckart J. Delirium and decisional incapacity in veterans with schizophrenia and medical illness. Gen Hosp Psychiatry. 2012;34:506-509.
4. Kahn DR, Bourgeois JA, Klein SC, Iosif AM. A prospective observational study of decisional capacity determinations in an academic medical center. Int J Psychiatry Med. 2009;39:405-415.
5. Cournos F. Involuntary medication and the case of Joyce Brown. Hosp Community Psychiatry. 1989;40:736-740.
6. Etchells E, Karz M, Shuchman M, et al. Accuracy of clinical impressions and Mini-Mental State Exam scores for assessing capacity to consent to major medical treatment: comparison with criterion-standard psychiatric assessments. Psychosomatics. 1997;38:239-245.
7. Appelbaum PS. Clinical practice: assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357:1834-1840.
8. Owen GS, Szmukler G, Richardson G, et al. Decision-making capacity for treatment in psychiatric and medical in-patients: cross-sectional, comparative study. Br J Psychiatry. 2013;203:461-467.
9. Merideth FL, Quinn DK. Walking the walk: decisional capacity deficits after right hemisphere subdural hematoma. Psychosomatics. 2016;57:102-106.
10. Dunn LB, Nowrangi MA, Palmer BW, et al. Assessing decisional capacity for clinical research or treatment: a review of instruments. Am J Psychiatry. 2006;163:1323-1334.
11. Etchells E, Darzins P, Silberfeld M, et al. Assessment of patient capacity to consent to treatment. J Gen Intern Med. 1999;14:27-34.
12. Sessums LL, Zembrzuska H, Jackson JL. Does this patient have medical decision-making capacity? JAMA. 2011;306:420-427.
13. Culver CM, Gert B. The inadequacy of incompetence. Milbank Q. 1990;68:619-643.
14. Masson N, Lester H. The attitudes of medical students towards homeless people: does medical school make a difference? Med Educ. 2003;37:869-872.
15. Geppert CM. Futility in chronic anorexia nervosa: a concept whose time has not yet come. Am J Bioeth. 2015;15:34-43.
16. Ganzini L, Volicer L, Nelson WA, et al. Ten myths about decision-making capacity. J Am Med Dir Assoc. 2005;6(3 Supple):S100-104.
Newsletter
Receive trusted psychiatric news, expert analysis, and clinical insights — subscribe today to support your practice and your patients.





