News
Article
The Role of Psychiatry in Advocating for Diverse Patient Populations in Primary Care Teams
Author(s):
How can consulting psychiatrists help the team provide culturally appropriate care for diverse patient populations?
Andrey Popov_AdobeStock

CASE VIGNETTE
“Brandon” is a 42-year-old divorced African American man with acquired hearing loss who has become unemployed recently due to layoffs during the COVID-19 pandemic. He has been admitted to the hospital for sepsis, and psychiatry has been consulted for agitation. Although it is in the early stages of the pandemic with a high rate of mortality, he has been asking members of the emergency medicine team to remove their face masks while caring for him.
The primary team is concerned that he is delusional because this seems unreasonable during a global pandemic. They place a behavioral flag on his medical record to notify other health care providers of a potentially dangerous patient. Although the patient has no psychiatric history, the team believes the patient’s behavior indicates a psychotic disorder, and they request recommendations for pharmacological treatment.
Brandon grew up without regular access to health care. As a child, he suffered from recurrent fevers that his family only treated with painkillers. The family later found out that Brandon had been getting ear infections, and the lack of treatment eventually led to permanent hearing impairment. He was born to 2 hearing parents who wanted him to be able to speak and lip read to fit into hearing society. They did not learn or use American Sign Language and chose for Brandon to receive a mainstream education.
As Brandon’s hearing has progressively decreased, he has found himself relying more on lip reading and facial expressions to follow conversations. With masking and social distancing during the COVID-19 pandemic, he has been afraid of losing even more of his autonomy and independence.
Brandon’s admission to the hospital has been a long and painstaking process. Since coming to the hospital overnight, he has spoken to multiple nurses and several emergency medicine physicians who have all been non-Latinx White. His evaluations occur after visitor hours are over, and due to the hospital’s COVID-19 policy, most interactions have been 1-on-1.
Although Brandon is comfortable speaking for himself, he has noticed that staff have an awkward demeanor around him. Because of past experiences of racism, he wonders if they are reluctant to interact with him because he self-identifies as Black. It has also been difficult to communicate with the team because the ambient noise in the emergency department interferes with his ability to hear what others are saying to him.
Discussion
How does Brandon’s intersectionality affect his experience of the health care system?
Brandon’s case highlights the complexity of patient experiences in health care. Health inequities are often discussed using single-identity categories such as race, gender, and sexuality. However, these categories interact with each other to affect how individuals experience their lives and interpersonal power dynamics.1 This is denoted by the concept of intersectionality—challenges that individuals experience may be better understood by considering their multiple identities at once as opposed to each category separately.2
In this case, aspects of Brandon’s social identity that may influence his care include his gender identity (male), his self-identified race (Black), and his disability status (hearing impaired). The care he receives may vary depending on clinician perceptions of the intersection of these identities.
Intersections matter: Black American men tend to have a higher rate of chronic physical illness than non-Latinx White Americans of any gender, and research shows it is the combination of race and gender that accounts for this difference.3 Literature review has also highlighted that the medical literature commonly conflates Blackness with genetics—meaning that the etiology of a particular condition is attributed to a biological cause rather than social construction of race, further fueling potential racism.4
How should the team balance the ethical dilemma of providing adequate care when they may have concerns about their personal safety during the pandemic?
Another consideration is the health care team’s personal safety during the pandemic. The clinicians seemed unwilling to make communication more accessible for Brandon due to the risk of their exposure to COVID-19. Although face masks can be a barrier to communication, removing them could indeed increase the likelihood that a health professional will contract COVID-19. However, clinicians have an ethical duty to provide equitable care.
Unconscious biases may influence the extent to which clinicians are willing to accommodate patients’ needs.5 In this case, the clinicians, being White and in a position of power and privilege in the hospital, may not have considered options such as moving Brandon to a quieter area. Instead, they reacted to Brandon’s requests with fear, assuming that he was dangerous or mentally ill.
At a systemic level, the Americans With Disabilities Act requires hospitals to provide effective communication with deaf and hard-of-hearing patients. However, hospitals often lack appropriate resources to support patients and may not provide assistive technology.6,7 Unfortunately, the early days of the pandemic highlighted that the US health care system did not have adequate resources to care for most patients.
Hospitals struggled to provide hospital beds to inpatients, ventilators to patients in critical condition, and adequate personal protective equipment to medical teams. This scarcity amplified the disparities in access to care that were already present. In addition, even experiences of vicarious racism during the COVID-19 pandemic have been shown to have negative impacts on mental health.8
In response to the pandemic and pervasive audism, the National Association for the Deaf has released guidelines for communication with deaf and hard-of-hearing individuals for hospital medical care and video-based telehealth services.9 In the hospital, using pen and paper is an option, but it is not ideal for gathering patient history, which requires multiple questions in succession.
In Brandon’s case, if the health care team had worn transparent face masks, this could have helped mitigate the conflict between effective communication and personal safety. Other examples of options for communication include video remote interpreting, speech-to-text, typing back, and captioned phone calls.
By asking Brandon for his preferred mode of communication, the team would have learned that he does not know sign language and a video interpreter would not have been helpful. Ensuring that he was roomed in an area with wi-fi could have empowered Brandon to have more autonomy if he had an internet-based app on his smartphone to assist with communication. There are both institutional and interpersonal elements of this case that highlight the phonocentricity of medical care.
Research has shown that psychiatric disorders tend to be more prevalent in individuals with hearing loss.10 Factors such as social isolation and loneliness may put patients at risk for mood disorders. Patients who are deaf or hard of hearing remain a population with unmet medical needs.11
What culturally appropriate recommendations can consulting psychiatrists provide for the primary team?
Consulting psychiatrists can help clarify the patient's experience through a clinical interview and advocate for the patient within the clinical environment. Sociocultural factors contributing to power differentials within interpersonal interactions need to be identified. A helpful mnemonic for this purpose is ADDRESSING,12 which stands for:
- Age and generational influences
- Developmental disability
- Disability acquired later in life
- Religion and spiritual orientation
- Ethnicity/race identity
- Socioeconomic status
- Sexual orientation
- Indigenous heritage
- National origin
- Gender
Consulting psychiatrists should help the primary team recognize and work effectively within these cultural differences. In addition to providing diagnostic clarification that the patient does not have a psychotic disorder, consulting psychiatrists can empathize with the primary team, offer a space for them to reflect on their pandemic fears, and help them recognize the pitfall of pathologizing behaviors that are appropriate responses to marginalization and discrimination.
Brandon's frustration becomes understandable in the context of racist and ableist oppression, and interventions should instead be focused on ensuring the provision of equitable care. By adopting a cultural lens, consultants can ensure that patients like Brandon have access to adequate supports while receiving appropriate medical treatment.
Consulting psychiatrists can direct the primary team toward resources included in the Table.
Table. Educational Resources That Consulting Psychiatrists Can Share With the Primary Team
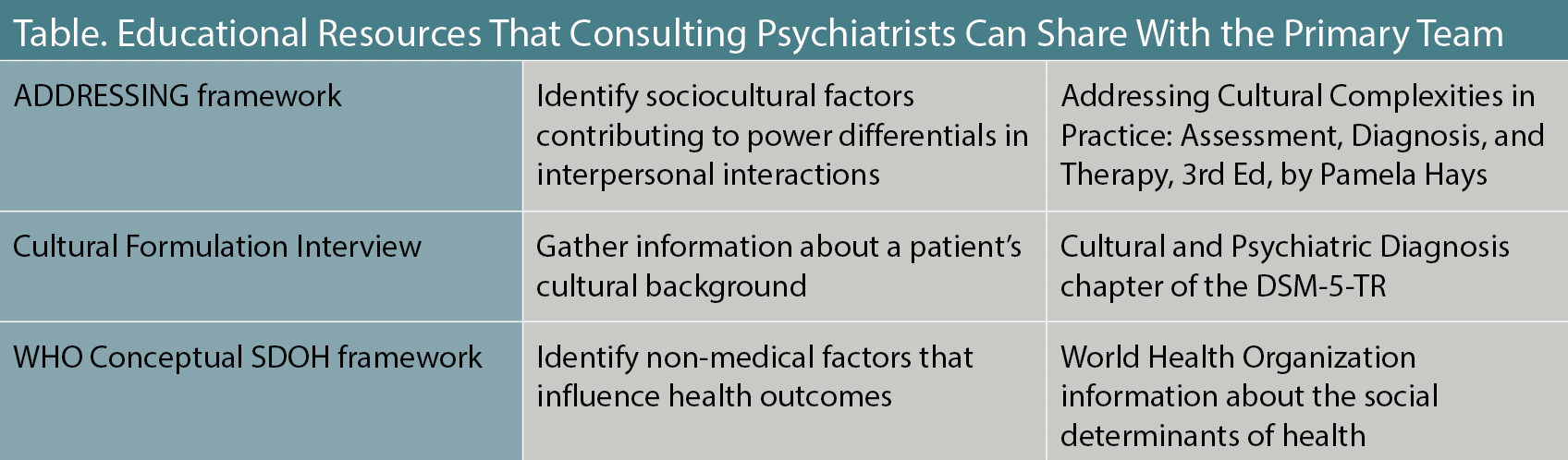
Further, psychiatrists may want to engage the team to conduct a comprehensive case formulation that takes cultural factors into account.
The American Psychiatric Association Outline for Cultural Formulation (OCF) is a framework that encompasses the domains of the cultural identity of the individual; cultural concepts of distress; psychosocial stressors and cultural features of vulnerability and resilience; cultural features of the relationship between the individual and the clinician, treatment team, and institution; and an overall cultural assessment.
To aid in the construction of a cultural formulation, the DSM-5 Cultural Formulation Interview was developed with standardized questions to help clinicians elicit and gather cultural information.13
Dr Wong (PGY-5) is an internal medicine-psychiatry resident at the University of California, Davis. Dr Fung is co-chair of the Group for the Advancement of Psychiatry (GAP) Cultural Psychiatry Committee and clinical director of the Asian Initiative in Mental Health.
Dr Lewis-Fernández is co-chair of the GAP Cultural Psychiatry Committee; a professor of clinical psychiatry at Columbia University; interim vice chair of research in the Columbia Department of Psychiatry; interim director of research at New York State Psychiatric Institute; director of the NYS Center of Excellence for Cultural Competence at NYSPI; director of the Hispanic Treatment Program at NYSPI; and research area leader for anxiety, mood, eating, and related disorders at NYSPI.
Dr Lu is a member of the GAP Cultural Psychiatry Committee and the former Luke & Grace Kim Professor in Cultural Psychiatry, Emeritus, at the University of California, Davis.
Note: The contributors have revised selected patient details to shield the identities of the patients/cases and to comply with HIPAA requirements. This column is meant to be educational and does not constitute medical advice. The opinions expressed are those of the contributors; they do not represent the authors’ organizations of employment and are not affiliated with GAP.
References
1. Ghavami N, Peplau LA. (2012). An intersectional analysis of gender and ethnic stereotypes: testing three hypotheses. Psychol Women Q. 2012;37(1):113-127.
2. Cooper B. Intersectionality. In: Disch L, Hawkesworth M. Eds. The Oxford Handbook of Feminist Theory. Oxford Academic; 2015.
3. Gilbert KL, Ray R, Siddiqi A, et al. Visible and invisible trends in Black men's health: pitfalls and promises for addressing racial, ethnic, and gender inequities in health. Annu Rev Public Health. 2016;37:295-311.
4. Cerdeña JP, Asabor EN, Plaisime MV, Hardeman RR. Race-based medicine in the point-of-care clinical resource UpToDate: a systematic content analysis. EClinicalMedicine. 2022;52:101581.
5. FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18(1):19.
6. Iezzoni LI, O'Day BL, Killeen M, Harker H. Communicating about health care: observations from persons who are deaf or hard of hearing. Ann Intern Med. 2004;140(5):356-362.
7. Stevens MN, Dubno JR, Wallhagen MI, Tucci DL. Communication and healthcare: self-reports of people with hearing loss in primary care settings. Clin Gerontol. 2019;42(5):485-494.
8. Chae DH, Yip T, Martz CD, et al. Vicarious racism and vigilance during the COVID-19 pandemic: mental health implications among Asian and Black Americans. Public Health Rep. 2021;136(4):508-517.
9. COVID-19: deaf and hard of hearing communication access recommendations for the hospital. National Association for the Deaf. 2020. Accessed March 15, 2024. https://www.nad.org/covid19-communication-access-recs-for-hospital/
10. Blazer DG. Hearing loss: the silent risk for psychiatric disorders in late life. Clin Geriatr Med. 2020;36(2):201-209.
11. Recio-Barbero M, Sáenz-Herrero M, Segarra R. Deafness and mental health: clinical challenges during the COVID-19 pandemic. Psychol Trauma. 2020;12(S1):S212-S213.
12. Hays PA. Addressing Cultural Complexities in Practice: A Framework for Clinicians and Counselors. American Psychological Association; 2001.
13. Aggarwal NK, Lewis-Fernández R. An introduction to the cultural formulation interview. Focus (Am Psychiatr Publ). 2020;18(1):77-82.
Newsletter
Receive trusted psychiatric news, expert analysis, and clinical insights — subscribe today to support your practice and your patients.






