
DSM-5 sleep-wake disorders are now more in sync with other medical disorders and sleep disorders classificatory systems. Here's what's changed.

DSM-5 sleep-wake disorders are now more in sync with other medical disorders and sleep disorders classificatory systems. Here's what's changed.

Here's a brief history of sleepwalking, associated factors, and pathology; sleep-related violence and forensic considerations; and management strategies.
Here's an update on parasomnias-the undesirable physical, experiential, or behavioral phenomena that occur exclusively during sleep onset, during sleep, or during arousals from sleep.

All psychiatrists know the risk factors for suicide. Among the newest modifiable risk factors to join the list are insomnia and nightmares.

Sleep disorders represent a significant problem in patients with Alzheimer disease. Here: assessment strategies and a review of drug and non-drug interventions.
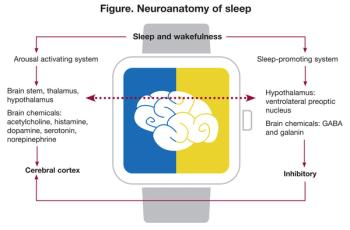
Sleep-related problems are among the most disabling consequences of TBI, with multiple influences: impairment of neuronal plasticity, metabolomic alterations, loss of vascular homeostasis, and disruption of the blood-brain barrier. The authors take a close look.

Here: the ordeal of a Russian psychiatrist who objected to the political abuse of psychiatry in the Soviet Union-and did something about it.
Despite the efforts of a dedicated Work Group, DSM-5 has not significantly changed the problems with PTSD that beset DSM-IV.

Do cholinesterase inhibitors lead to weight loss in older adults with dementia? Here's a wrap up of a large study of patients in a real-world setting who had newly started these medications.

Twenty years ago, it was rare for college students to mention suicidal thoughts, and even more rare to involve parents in their care. Today, students are more likely to describe suicidal ideation, necessitating a more thorough safety assessment with potential outreach to parents.

A look at what neuroimaging studies reveal, methylation patterns of the NR3C1 gene, and new methods to address disturbances in the parent-child relationship.

How will mobile mental health technologies change the nature of the psychiatrist-patient relationship? And do these technologies truly deliver what they promise?

Here: practical tips on how to proceed with the treatment recommendation process with families who prefer therapy alone.

Potentially over-inclusive DSM-5 diagnostic categories for somatic disorders can result in a confusing overlap of criteria. These authors sort through the challenges of the differential diagnosis-and map out a well-structured treatment plan.

Details here about a protocol for opioid abusers and the mentally ill that helped avoid deaths from drug overdose after psychiatric hospitalization.

Ronald Pies, MD reviews the second edition of Ansari and Osser’s overview of psychopharmacology.

The story is decades old, but it reverberates today -- incidents of police brutality and excessive force, sometimes lethal. Here's a psychiatrist's story of serving on a citizen's review committee in Houston back in the day.

Don't miss the June 28th issue of the New York Times magazine with a special series on psychiatric issues that illustrate for general readers some of the most important - and exciting - advances in our field.

He smoked trabucos, mild miniatures produced by the Austrian monopoly, but preferred Don Pedros and Reina Cubanos...
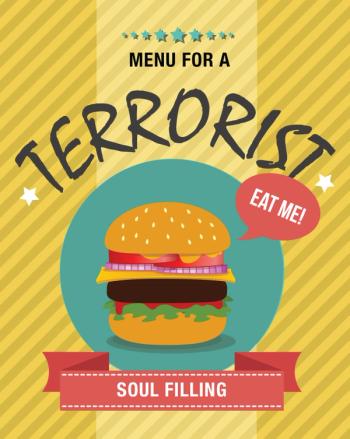
The authors explore possible reasons why young people in the West leave their families, friends, and home culture to join terrorist organizations.

Experts summarize data on the role of inflammation in psychiatric disorders, emphasizing that evidence for anti-inflammatory treatment for mood disorders is limited, and mixed.
A recent study from the Bipolar-Schizophrenia Network on Intermediate Phenotypes (B-SNIP) investigated the genetics of the auditory event-related potential, a putative psychosis biomarker.

Researchers have identified a “multiple-deficit” model of the comorbidity between ADHD and dyslexia in which each disorder has multiple predictors-some specific and some shared.

"The time is right to use research-informed interventions and implementation strategies to address the quality chasm for mental health care," says to NIMH Director Insel.

Unspecified bipolar disorder? Comorbid borderline personality disorder? Or, in the case presented here, is it time to break out the mixed specifier from DSM-5?