
The goal of palliative care is to prevent and relieve suffering and to improve quality of life for people facing a serious, complex illness.

The goal of palliative care is to prevent and relieve suffering and to improve quality of life for people facing a serious, complex illness.

An Overview of Antipsychotic Use in Older Adults

Who should care about aging? This question is particularly germane in mental health. The articles in this Special Report remind us of the importance of understanding and focusing on the stresses, problems, and treatment-related issues in this population.

Opioid Dependence and XR Naltrexone

Adolescents with ADHD, conduct disorder, or who smoke cigarettes are less likely to finish high school on time and more likely to drop out altogether, researchers at the University of California, Davis, School of Medicine have found.

A joint study by researchers at two universities reported that the majority of people with alcohol problems who seek out clergy for help have or will also use professional mental health services at some point in their recovery process.

Is there a link between heartbreak and addiction? A recent study shows that the same areas of the brain were affected as those associated with addiction, reward, craving, and depression.

Decreasing the Clinician’s Risk

As with all medical emergencies, psychiatric emergencies are among the most clinically challenging situations.

I offer all of this as a way of describing how I became involved in intensive psychotherapeutic efforts with several adolescents who I then continued to see, often for many years following their inpatient experiences.

Fads in psychiatric diagnosis come and go and have been with us as long as there has been psychiatry. The fads meet a deeply felt need to explain, or at least to label, what would otherwise be unexplainable human suffering and deviance.

From 19th century French impressionists to current-day “rockers,” it has always been a loosely held belief that creative genius encompasses (even embraces) substance use. But a recent study found that substance use impedes artistic creativity.

As early as the 1970s, researchers and practitioners became increasingly aware of the necessity for services that would address the varied needs and treatment implications for consumers with the co-occurring disorders of substance abuse and mental illness. High percentages of consumers in substance abuse treatment centers were identified with mental illness disorders, and consumers admitted to psychiatric facilities often were identified as having additional substance use disorders.

When I was an undergraduate studying molecular biology in the early 1990s when the Human Genome Project had just begun, my required coursework included several lectures on the ethical implications of sequencing, understanding, and ultimately being able to manipulate the “code of life.”
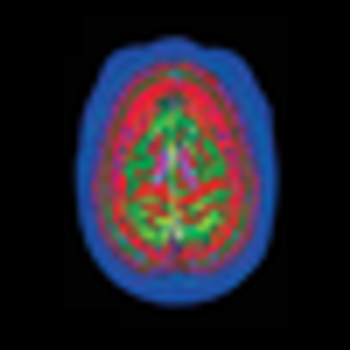
The causes of Alzheimer disease and attempts to predict who is at risk for it have been confounding the medical profession ever since Dr Alzheimer first described the disorder in 1906. Finally, a breakthrough in dye and imaging technology may be the key to solving the puzzle.

Professor Hannah Decker, a distinguished historian by trade, has posted a thorough, fair, and sprightly history of the DSM5 controversy. We are all lucky to have her as chronicler.

Consider these 2 scenarios:

Ethical Questions at the Intersection of Neurotechnology and Psychiatry

Avoiding Confidentiality Conflicts

Dramatology approaches human encounters, events, and scenes as dramatic enactments of characters in conflict and crisis.

Almost the first memory I have of a physician is our family doctor at my bedside, leaning over to press his warm fingers against my neck and beneath my jaw. I’m 5, maybe 6 years old. I have a fever and a sore throat, and Dr Gerace is carefully palpating my cervical and submandibular lymph nodes.

Questions have also been raised about the extent of industry influence on the American Psychiatric Association’s diagnostic and treatment guidelines-namely, its DSM and Clinical Practice Guidelines.

DSM5 first went wrong because of excessive ambition; then stayed wrong because of its disorganized methods and its lack of caution. Its excessive and elusive ambition was to aim at a “paradigm shift.” Work groups were instructed to think creatively, that everything was on the table. Accordingly, and not surprisingly, they came up with numerous pet suggestions that had in common a wide expansion of the diagnostic system-stretching the ever elastic concept of mental disorder. Their combined suggestions would redefine tens of millions of people who previously were considered normal and hundreds of thousands who were previously considered criminal or delinquent.

The recently posted criteria sets for DSM5 are a mess. The writing is unclear, inconsistent, and imprecise. Unless they are edited and drastically improved, any field testing based on them will be a waste of time, effort, and money- and DSM5 may not be usable.

I am writing to commend Flavie Waters, MD, for her recent article on auditory hallucinations in psychiatric illness.1 She covers the topic well. Her article is timely and I hope it will contribute to a badly needed reorientation of our field toward the positive symptoms of schizophrenia. However, I am compelled to point out an error of citation that is not the author’s fault.