
Sex and gender, influenced by genetics, epigenetics, and environmental/social stressors, must be considerations in evaluating every patient.

Sex and gender, influenced by genetics, epigenetics, and environmental/social stressors, must be considerations in evaluating every patient.

Catch up on all the latest in psychiatric comorbidities.
30% to 60% of individuals seeking treatment for SUD also meet criteria for PTSD.

The average patient with bipolar disorder struggles with sleep disorders. Here's how you can help.
Comorbidity: The concept is simple enough, but in practice, comorbidity drives complexity and presents the specters of diagnostic ambiguity and therapeutic unpredictability.


Put treatment resistance in perspective with Sheldon H. Preskorn, MD.

Collective trauma: psychiatry can play a major role in addressing public anxiety and fear.


Women are currently facing a number of important issues in mental health. How can clinicians improve this situation?
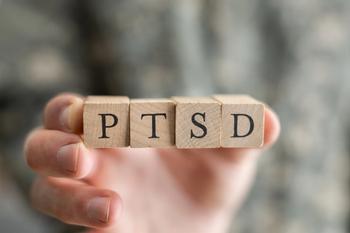
Trauma-related psychiatric disorders such as PTSD and grief often go undetected and untreated in older adults. Here's how to help.

What sleep disorders are common in older adults and what are the associated risk factors and correlates?


Autism spectrum disorder often evades formal diagnosis until a child is 4 years or older, but these artificial intelligence and telehealth systems may be able to help facilitate diagnosis.

A well-being centered approach expands assessment and treatment for the child’s strengths and opportunities for positive experiences with the family.

Television, tablets, gaming, phones: how are they impacting child and adolescent mental health?


Each Native American tribe has a specific history, traditions, customs, and culture, and knowing something of these will help build the physician-patient relationship.

Women experience depression at rates twice that of men. But Black women are only half as likely to seek care as White women. Here's what you can do to help this population.

Understanding a patient's sociocultural background will have an important effect on treatment, especially for Hispanic patients.

The rise in anti-Asian violence will likely lead to a rise in Asian Americans presenting for psychiatric care. Here is how best to address the longer-term problems they face...

By recognizing the importance of minority mental health and caring for all types of patients, psychiatrists depict the epitome of humanity.

Due to discrimination's negative impact, transgender and gender-nonconforming youth are several times more likely than the rate of their cisgender peers to have depression and anxiety.

Online environments have revolutionized the lives of young SGM individuals, but also created unforeseen issues...

What academic terminology should be used when describing sexual and gender minority patients?

Homosexuality was classified as a mental illness until 1973. We have come a long way, but there is a lot further to go...

The sexual side effects of psychiatric medications are troubling enough that some patients consider treatment cessation. The authors review 5 strategies for managing sexual dysfunction.
Sedation may not always be desirable, but it is difficult to avoid in psychiatry. Some of the most sedating medications are discussed.

Antipsychotic-induced weight gain evolves over time, leads to chronic complications, and is very difficult to reverse. Pharmacologic interventions used to tackle weight gain are modestly effective and worth considering in certain cases.