
Placing black floor mats in front of exits to deter demented nursing home residents from dangerous wandering may pose ethical questions.

Placing black floor mats in front of exits to deter demented nursing home residents from dangerous wandering may pose ethical questions.

Which of the following complementary and alternative medicine (CAM) therapies may have beneficial effects on symptoms of mild cognitive impairment (MCI) and Alzheimer disease (AD)?

Mental illness is a risk factor for HIV infection. It brings a number of behavioral correlates that put patients at risk for getting infected. As HIV infection worsens, it begins to affect the brain, and cyclical relationship between the disease and mental illness begins.

Less common but still important syndromes connected with Alzheimer disease include traumatic brain injury, infectious and inflammatory disorders, alcohol-induced dementia.

Psychiatric disorders, such as primary sleep disturbances, depression, substance abuse, mania, sexually inappropriate behaviors, and psychosis, can complicate the care of patients with dementia.

The goal of this article is to improve recognition of comorbid psychiatric and movement disorders and to help the reader formulate a management strategy using a multidisciplinary approach.

The number of medical diseases that can present with psychotic symptoms (ie, delusions, hallucinations) is legion. A thorough differential diagnosis of possible medical and toxic causes of psychosis is necessary to avoid the mistaken attribution of psychosis to a psychiatric disorder.

When this physician published an article containing his case summaries of 3 women with dementia praecox, he made it clear that this was a disease that neurologists and physicians in general practice could easily and reliably diagnose by following his diagnostic procedures.

Of the 3 informative articles included in this special geriatric collection, 1 offers a perspective on the treatment of depression that does not focus on somatotherapy. The others remind us of 2 additional geriatric Ds of importance: drugs and driving.

Medical professionals may be reluctant to initiate a discussion about driving with older patients in anticipation of a negative impact on the physician-patient relationship.

Age is a major risk factor for the development of Alzheimer disease and other dementias. New technologies in brain imaging represent major advances in our ability to diagnose age-related cognitive and behavioral disorders.

Although the adverse-effect profile of older, conventional (typical) antipsychotics has discouraged many clinicians from using them, they remain widely used in elderly patients with dementia.

Research is needed to define clinical biomarkers and genetic screens that could be used to identify early stages of dementia and to link clinical syndromes with the later development of dementia.

Anton Porsteinsson, MD, discusses some specifics for fine-tuning the care of patients with Alzheimer disease. Here: optimizing physical health and mental stimulation and promoting a brain-healthy diet and aerobic exercise.

Can stimulants increase function in people with early stage Alzheimer disease? Here, Anton Porsteinsson, MD, discusses the pros and cons.

The team approach to dementia psychiatry services requires leadership for direction, decision making, and policy changes in order to make the process efficient and beneficial for all involved.

Do patients with the personality trait alexithymia have trouble understanding the written language? What percentage of patients with dementia have at least one psychiatric comorbidity? These and more in this quiz.

As I lie in my hospital bed, attempting to breathe through my trach tube at a normal rate, waiting for my morning medication, and hoping to hear good, or at least manageable, results from my doctors when they come to me on rounds, my mind wanders. Despite the precariousness of my situation, I can’t help but smile as I think of my now monthly psychotherapy sessions.

Focus on Obesity, Insulin Resistance, and the Metabolic Syndrome

Since the early twentieth century, when Alois Alzheimer and Emil Kraepelin constructed it as a unified clinical-pathological entity, Alzheimer’s disease has been both one of the most stable and one of the most problematic neuropsychiatric entities.

Keys to diagnosis, assessment, and management.
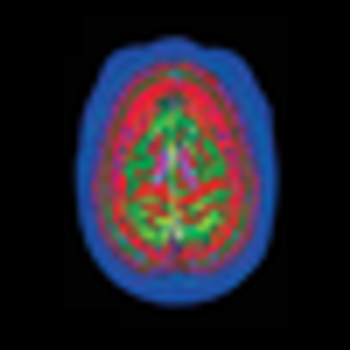
The causes of Alzheimer disease and attempts to predict who is at risk for it have been confounding the medical profession ever since Dr Alzheimer first described the disorder in 1906. Finally, a breakthrough in dye and imaging technology may be the key to solving the puzzle.

Resources, books, and practice guidelines

This article reviews the differences between dementia types and future directions.

The United States Census Bureau projects that by 2010 nearly 13% of the US population will be over the age of 65. The elderly are one of the most rapidly growing segments of the US population and are expected to account for more than 20% of the total population by 2050.1 In 2001, the prevalence of dementia in North America was 6.4%. A 49% increase in the number of people with dementia is expected by 2020, and a 172% increase by 2040.2 Patients with dementia may lack the capacity to consent to treatment. The need to evaluate capacity to consent to treatment will therefore increase as the aging population grows.