
This hormone-based therapy shows promise for older women with refractory symptoms.

Dr Miller is professor in the Department of Psychiatry and Health Behavior, Augusta University, Augusta, Georgia. He is on the Editorial Board and serves as the schizophrenia section chief for Psychiatric Times. The author reports that he receives research support from Augusta University, the National Institute of Mental Health, and the Stanley Medical Research Institute.

This hormone-based therapy shows promise for older women with refractory symptoms.

What should you tell your patients with schizophrenia about exercise?

Insights from the first study of mortality and cumulative psychotropic exposure in schizophrenia.

New insights from a large study that relied on objective biomarkers.

What is the risk of symptom recurrence after antipsychotic discontinuation in first-episode psychosis?

What role does DNA methylation play in schizophrenia?

Details of a randomized trial of an alpha-7 nicotinic receptor agonist in schizophrenia.

Is clozapine still the gold standard for treatment-resistant schizophrenia?

Do atypical antipsychotics increase the risk of major malformations among exposed infants?
The identification of a genetic risk factor has shed light on the underlying neurobiology of the disorder.
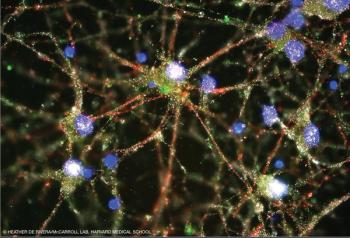
Groundbreaking work by a Harvard team represents a bold step in our journey toward understanding schizophrenia.

Brain-based biomarkers identify more biologically homogeneous categories of psychosis than do clinical diagnoses.

Are you up-to-date on the risk of recurrent pneumonia in patients with schizophrenia when an antipsychotic is reintroduced?

New evidence-coupled with advances in molecular biology-has afforded an unparalleled opportunity to move toward identifying potential new treatments for schizophrenia.

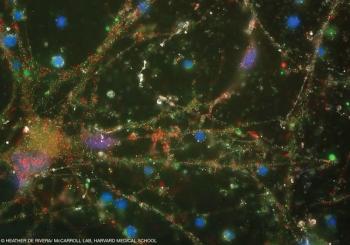
Neuroinflammation may be a culprit in the development of psychosis. What are the clinical implications?

How targeted interventions may reduce the burden of premature mortality among patients with schizophrenia and other psychiatric disorders.

The first episode of psychosis represents a critical juncture in the treatment of schizophrenia. Here: A synopsis of 2-year outcomes from the NIMH Recovery After an Initial Schizophrenia Episode (RAISE) Early Treatment Program.

Information about the performance of clozapine compared with other treatment strategies in usual practice may impact on its use in routine clinical settings. Here: findings from US national Medicaid data in a cohort of patients with treatment-resistant schizophrenia.

The abuse of alcohol by patients with schizophrenia is a remarkably common phenomenon. Here: findings from a 6-month randomized trial of long-acting injectable versus oral risperidone in patients with schizophrenia and comorbid alcohol use disorder.

Treatment with a selective estrogen receptor modulator in adjunct to antipsychotics was associated with improvements in attention and memory in men and women with schizophrenia in a recent trial.
A recent study from the Bipolar-Schizophrenia Network on Intermediate Phenotypes (B-SNIP) investigated the genetics of the auditory event-related potential, a putative psychosis biomarker.

We are in the midst of a paradigm shift in the field, and new diagnostics and treatments that yield clinically significant improvement for the heterogeneous set of disorders known as schizophrenia are being developed.

A paradigm-shifting finding holds the potential to alter how we perceive brain-immune interactions for disorders like schizophrenia and Alzheimer disease. It would enable a more mechanistic approach to the study of the neuroimmunology of these and other disorders.
A new network-based neuroimaging study seeks to identify biomarkers across the spectrum of impairment in schizophrenia.

The authors review the evidence for the use of ECT and other novel neurostimulation techniques in the treatment of schizophrenia.

Take-home messages on the immunology of schizophrenia and NMDA receptor encephalitis from the Schizophrenia International Research Society conference here.

There is renewed interest and enthusiasm for the potential pathophysiological role of inflammation and immune dysfunction in patients with schizophrenia, with evidence for abnormalities in the blood, CSF, and CNS.

How frequently do you find yourself prescribing antibiotics for inpatients with schizophrenia and related psychotic disorders during hospitalization?