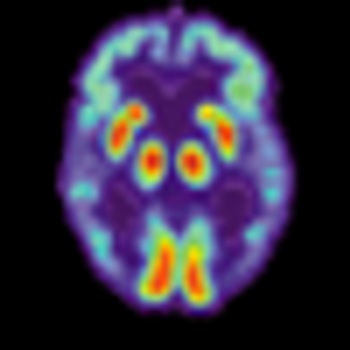
If telling patients they have “pre-clinical Alzheimer’s” or “MCI due to Alzheimer’s Disease”-absent effective treatment-produces more emotional suffering than it relieves, a difficult ethical question arises; namely, can such a disclosure be justified under the foundational principle of non-malfeasance?














