
News


What Every Psychiatrist Needs to Know to Be Prepared

Decreasing the Clinician’s Risk

Keys to diagnosis, assessment, and management.

As with all medical emergencies, psychiatric emergencies are among the most clinically challenging situations.

Is there growing evidence suggesting that paternal depression is associated with interpersonal problems with the mother and maternal depressive symptoms? Can severe psychiatric disturbances result from paraneoplastic disorders? Find out the answers to these questions in this week's quiz.

After years of war, more and more Iraquis are seeking medical care for trauma-induced mental illness. However, demand for such treatment far outpaces supply. In a country of 30 million people, only 100 psychiatrists are available to offer care.

Business groups and leading behavioral managed care companies have mounted a multifront attack on the new mental health parity law. The Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act (MHPAEA) went into effect on January 1, 2010, for employer plans starting after that date. However, companies have been awaiting a delayed final rule interpreting the terms of the MHPAEA.

I offer all of this as a way of describing how I became involved in intensive psychotherapeutic efforts with several adolescents who I then continued to see, often for many years following their inpatient experiences.

As many as 80% of patients who use herbal preparations and other natural products regard these therapies as the primary treatment of their ADHD symptoms.

Ultimately, Dr Ghaemi endorses a pluralistic approach and a “method-based psychiatry” in contrast to the eclecticism of the BPS. This method-based approach recognizes that one method may be more correct than others on the basis of empirical data and conceptual soundness (the “less is more” view), versus the BPS model, in which all methods can be equally correct (the “more is better” view).

I can still hear the click of clue tiles

It is rather difficult for me to avoid turning this greeting article into an homage to Dr Pies. My mirroring of his farewell piece2 with my title and preliminary quotes was meant to signify my great respect for him. How much I have learned and benefited from his wisdom, patience, knowledge, and compassion over the past 4 or so years cannot be measured.

Many Americans seem angry at President Obama’s seeming lack of anger over the BP fiasco. Frustration with the environmental calamity in the Gulf is perfectly understandable. Anger with those who should have foreseen and prevented this horrendous situation is also understandable, and-up to a point-quite justifiable.

A recent study reports that only a small fraction of substance abuse treatment facilities provide specialized services for the lesbian, gay, bisexual, and transgender community, and that the majority of those are privately run.

Fads in psychiatric diagnosis come and go and have been with us as long as there has been psychiatry. The fads meet a deeply felt need to explain, or at least to label, what would otherwise be unexplainable human suffering and deviance.

According to physician recruiters Merritt Hawkins, result comparisons between 2006/2007 and 2009/2010 surveys reveal a 121% increase in requests for psychiatrists. And the US Bureau of Health Professions predicts a 100% rise in demand for psychiatrists by 2020.

It is probably self-evident that to be a celebrity doctor requires at the minimum certain characteristics. The doctor needs to be comfortable being an authority figure and, at the same time, convey humanistic concerns. Being telegenic helps if you are on television a lot.

The limited empirical research evidence supports the impression that practitioners, if they use the manuals at all, use them in a loose, informal manner and are comfortable ignoring diagnostic criteria and making their diagnoses following an informal prototypal pattern.

Why not define mental disorder just on the presence or absence of the characteristic cluster? Why was it felt to be necessary to also require distress or impairment?


Every month or so, someone (usually very smart and passionate) sends me a detailed proposal for a new diagnostic system offered as an alternative to the jumbled, pedestrian, atheoretical, and purely descriptive method used in DSM.

Test your psych knowledge with our weekly quiz highlighting content from Psychiatric Times and around the Web.

From 19th century French impressionists to current-day “rockers,” it has always been a loosely held belief that creative genius encompasses (even embraces) substance use. But a recent study found that substance use impedes artistic creativity.

As early as the 1970s, researchers and practitioners became increasingly aware of the necessity for services that would address the varied needs and treatment implications for consumers with the co-occurring disorders of substance abuse and mental illness. High percentages of consumers in substance abuse treatment centers were identified with mental illness disorders, and consumers admitted to psychiatric facilities often were identified as having additional substance use disorders.

When I was an undergraduate studying molecular biology in the early 1990s when the Human Genome Project had just begun, my required coursework included several lectures on the ethical implications of sequencing, understanding, and ultimately being able to manipulate the “code of life.”
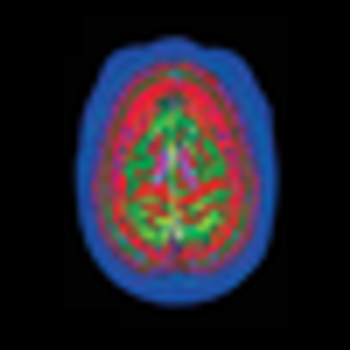
The causes of Alzheimer disease and attempts to predict who is at risk for it have been confounding the medical profession ever since Dr Alzheimer first described the disorder in 1906. Finally, a breakthrough in dye and imaging technology may be the key to solving the puzzle.

Professor Hannah Decker, a distinguished historian by trade, has posted a thorough, fair, and sprightly history of the DSM5 controversy. We are all lucky to have her as chronicler.

The effects of the BP oil spill are sure to reach beyond the environment. Psychiatrists warned that the spill may have long-term psychological consequences on residents, mental health workers, and cleanup volunteers.

With Medicare reimbursement cuts looming, many physicians are considering opting out of Medicare. And it’s not just payment rates that have doctors dropping out: those who participate in Medicare are struggling to cut through the red tape just to keep their coverage active.