
A review of some of the latest study findings on the pharmacological treatment of prodromal psychosis.

A review of some of the latest study findings on the pharmacological treatment of prodromal psychosis.

Here, Dr Jon E. Grant talks about the genetics, neurobiology, and cognitive processes of body-focused repetitive behaviors, which include trichotillomania, skin picking, and other behaviors.

What role do you play in managing stalking behaviors? How can you read between the lines and determine which stalker type behavior a patient's communication suggests?

Here, Debra Pinals, MD, looks at the development of anti-stalking legislation, the epidemiology of stalking, and various stalking classification schemes from a clinical perspective.

Here, John Femia, a former police officer and senior investigator, describes his experience as a first responder to scenes of violence and stalking. He offers a profile of those who stalk others; describes different types of stalkers; and focuses in on cyberstalking-all with the mental health clinician in mind.

Randi K. Bregman, LMSW, is the Executive Director of Vera House, Inc. (http://www.verahouse.org/). In this video, she talks about the impact of trauma and violence as defining forces in the lives of those who have been abused.

At the 3rd Annual Forensic Psychiatry Conference in Syracuse on August 11, retired FBI agent Robert (Roy) Hazelwood, MS, discussed how ritualistic serial rapists are distinguished from other rapist populations.

In this final of a 3-part podcast series, Brian Smith, MD, discusses the how’s, the why’s, and the treatment options for adolescents who harm themselves.

That unusual topic was addressed by Dr Eugenio Rothe at a symposium at the recent APA meeting in Honolulu.

Might your patient be feigning mental illness? Forensic psychiatrist Phillip Resnick, MD offers insights.
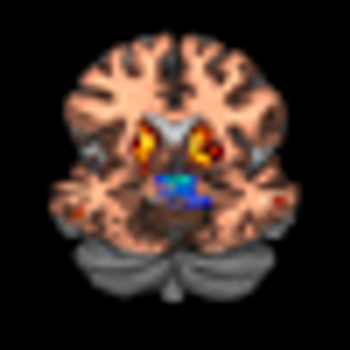
How can we combine neuroscience and psychotherapy to best serve patients with psychiatric disorders?

In Part 2 of this podcast series, Dr Smith continues his discussion of the practice of nonsuicidal self-injury in adolescents.

In this podcast, Dr Smith discusses the practice of nonsuicidal self-injury in adolescents-cutting, burning, self-hitting or banging, scratching, interfering with wound healing-may be increasing.

In the second in his series of podcasts, Dr Phillip Resnick answers questions psychiatrists often ask about assessing the risk of violence.

In the first in a series of brief podcasts, Dr. Phillip Resnick answers questions often asked about assessing risk for suicide and violence.

The efficacy of psychodynamic psychotherapy is supported by empirical evidence. Patients have reported residual therapeutic gains following treatment.

In this podcast, Dr Caine discusses the many issues associated with suicide and touches on specific articles in this Special Report.

America, it seems, is shy about 45,000 psychiatrists. That’s the premise of a controversial article entitled “45,000 More Psychiatrists Anyone?” by Dr Dan Carlat, that was published in the August 2010 issue of Psychiatric Times….and it’s that article that Dr Sidney Weissman has chosen as his Top Paper of the Year.

More than half of parents who have children with ADHD treat their child’s symptoms with vitamins, dietary changes, and expressive therapies-but only a small minority tell their doctor. More in this podcast.

The federal government is urging hospitals, physicians, and other healthcare stakeholders to collaborate for better patient care and smaller medical costs through accountable care organizations (ACOs). But with Washington, D.C., still undecided about what ACOs will look like, physicians nationwide are left wondering about their roles in this new initiative.

Dr David Osser has chosen as one of the Top Papers of the Year a meta-analysis on second generation antipsychotics and the effects of these agents on patients with schizophrenia.

A meta-analysis sheds new light on the safety and efficacy of antidepressants in the acute treatment of bipolar disorder.

With the availability of drugs for ADHD and Alzheimer disease, more and more healthy people who have no mental health condition have been asking their psychiatrist to prescribe neuroenhancing medications in the hopes of improving their memory, cognitive focus, or attention span. What's an appropriate response when one of your patients asks for a prescription for a drug for this off-label purpose?

Since the 1980s, there have been growing concerns that chronic cholesterol depletion may actually increase noncardiovascular deaths by suicide and violence-related deaths.

Is combination therapy with lithium and valproate more effective in preventing relapses in patients with bipolar I disorder than monotherapy with either drug alone?

Olfactory reference syndrome (ORS) may be more common than generally recognized, according to Dr. Katharine Phillips-a leading expert on this disorder.

Some psychiatrists include “testimonials” from their patients on their web sites. Such recommendations are a major source of new referrals. . .but is this an ethical way of promoting my clinical services?

Like millions of Americans, I’ve joined Facebook. I really enjoy it because it conveniently lets me stay in touch with my friends. I don’t tell my patients that I have a Facebook profile, but many patients tell me about their Facebook activities during therapy. How should I respond if a patient to “friend” me?

I’m one of the only psychiatrists practicing in this area. What am I realistically supposed to do when I see one of my patients in public? Whenever I go to the gym or library or grocery store, I see several patients I’m actively treating. Some want to say hello and some want to socialize. My response so far has been to try to avoid them.

One of the country's leading experts on career development offers guidance on job resources; on practicing alone, in a group or clinic or hospital, or in a government facility; on presenting your academic credentials most effectively; on locum tenens practice; on consulting for insurance companies or Medicare; and on alternatives to full time practice.