
Michelle Riba, MD, shares her thoughts on the days ahead.

Michelle Riba, MD, shares her thoughts on the days ahead.

Ronald Pies, MD, offers advice on talking to patients about spirituality during the COVID-19 pandemic.

Virtual happy hours abound, but this is also quite worrisome, especially for those struggling with alcohol and substance use. Alternative solutions are offered in this video.

While anxiety, depression, loneliness, substance abuse. and domestic violence are inevitable consequences of physical isolation and reduced socialization from coronavirus, emotional strain is not limited to COVID-19.

Behavioral health care providers are needed now more than ever to help support frontline caregivers and to provide access to care. Deena Tampi, MSN, MBA-HCA, offers insights about caring for the caregiver as well as providing access to care.

Rajesh R. Tampi, MD, MS, DFAPA, provides guidance for frontline health professionals and caregivers to mitigate stress and burden.
How can psychiatrists help caregivers deal with behavioral disturbances at home, without the possibility of an in-person doctor’s appointment? In this video, Marc E. Agronin, MD, offers tips for helping patients with Alzheimer disease and other dementias.

Tips for advocating for yourself and the safety of your patients.

Allen Frances, MD, delivers a powerful message for mental health professionals to help them navigate the COVID-19 pandemic.

Within days of the COVID-19 pandemic, students scattered from campus to locations around the country, and their psychiatric care was interrupted at a time when they needed support more than ever.

It is one thing to hear from colleagues about how patients and the public are coping with the pandemic. It is quite another to hear directly from children. Five-year-old Adam, his parents, and I invite you to join Team Earth. Here’s why.

"Mom says viruses don’t attack countries, they attack people. And across countries we are still one people living under one roof." More in this pictorial and therapeutic dialog between a 5-year-old and his mother about the pandemic.

What is a “normal” reaction to this pandemic? How does one adapt to a new normal? How does an organization that has to downsize drastically adjust successfully, especially after the “honeymoon period”?
Dr Jud Brewer discusses the benevolent effects of altruism during the coronavirus pandemic in this brief podcast.

As we face a medical and existential crisis, how do we find strength and cope with stress and trauma? A podcast with Ronald W. Pies, MD.

Clinicians work with more male sexual abuse survivors than they may think.

Three mountains must be climbed to emerge unscathed.

An overview of the theoretical and empirical literature linking PTSD, substance use, and IPV, as well as risk factors for depression and other psychiatric disorders.
Health professionals' emotional reactions to the COVID-19 pandemic range from numbness, anxiety, fear, and rapid shifts to survivor guilt, helplessness, and feelings of detachment. Here: Stress management tactics and what to expect today and beyond.

Most of us remember where we were when the terrorist bomb shattered our sense of peace in this usually quiet community. The shockwave travelled for miles and across time.
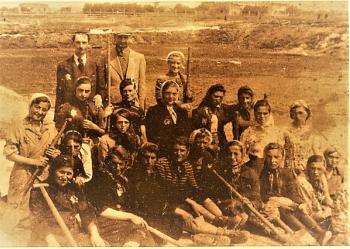
For an inspiring model of communal hope and resilience under a dire threat to survival over COVID-19 fears, the author turns to the Fekalists, the prisoners condemned to be sanitation workers in the Lodz ghetto in Nazi-occupied Poland, his parents among them.

As our understanding of the neurobiology of OCD grows, additional treatment options become available and should be thoughtfully integrated into the treatment algorithm. One such option is dTMS.

Sit back and listen to Dr Jud Brewer discuss integrative approaches to managing anxiety during the COVID-19 pandemic.

In these uncertain times, many look to Franklin D. Roosevelt’s quote “The only thing we have to fear is . . . fear itself.” But what does that really mean?
So begins this transformative journey to calm, peace, and tranquility in the face of a “coronacopia” of life upending challenges.