
As physicians first, psychiatrists must consider the big picture, without reflexive and thoughtless prescriptions for psychotropics—even if many, including medical professionals, assume that is all we do.

As physicians first, psychiatrists must consider the big picture, without reflexive and thoughtless prescriptions for psychotropics—even if many, including medical professionals, assume that is all we do.

This case illustrates the practical implications and effectiveness of the Minnesota Multiphasic Personality Inventory-2 in documenting patient recovery during treatment for delusional disorder.
A 59-year-old man with a history of multiple concussions has been having a series of neurocognitive symptoms for the past several years. Discover more in this case.
Lack of empathy is a commonly known feature of narcissistic personality disorder. Relationships are typically shallow and difficult to maintain. What are some other features of NPD? More in this case presentation.

James L. Knoll IV, MD, analyzes the ethical and legal duties of psychiatrists treating substance use disorders.

The costs, risks, and considerations involved in treating addiction have upped the ante, as illustrated in this case.
Doing a review of systems wasn’t “rocket science,” as they say-but it was a classic example of medical science and of why psychiatrists are physicians first.

The reported severity of the complaints in this patient appears grossly out of proportion given gathered information and clinical observations. What's your diagnosis?
Providing detailed descriptions of interactions that occurred between patient and therapist moved our field forward by both honing our technique and considering more effective ways to help our patients. But is the sharing of cases ethical?

When, if ever, is it ethical to administer a medication to a patient-even an incapacitated one-without his knowledge? Read the case, and weigh in.
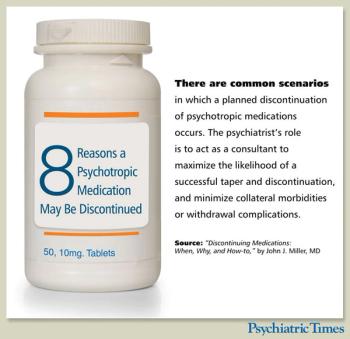
Tips for having a balanced and comprehensive risk-to-benefit discussion with competent patients who want to stop their medications.

What factors predispose patients to TRD and what treatment strategies achieve response? Find out here, with a bonus case vignette.

Got a challenging case-a patient for whom the diagnosis is unclear or uncertain? Want a diagnostic opinion? This is a call for cases. Michael First, MD-a nationally recognized expert on psychiatric diagnosis and assessment issues-will review details and offer insights on select cases.

Your patient is excited to be pregnant. She is currently on sertraline, and has been stable on this for many years. She is very insistent that she would like to stop her medication. What should you do?
“Googling” a patient does not seem much different from the old-fashioned obtaining of collateral information, but the ramifications may be far more than you bargain for.

Does this patient have decision making capacity to refuse a blood transfusion that will likely save his life? You are the ethics consultant, and the decision is yours.
Ethics case quiz: A patient's inconsistent decisions regarding treatment are cause for concern. What to do?
Psychiatrists increasingly recognize that not all treatments for depression are created equal-but in this case, an entirely different diagnosis came to light.

A reminder that success in life requires paying attention to the basics, starting with showing up and hanging in there.
Renal failure is not an uncommon disorder either in the general public or in patients with psychiatric disorders, but accompanying depression, anxiety, and loss must be attended to during such an illness.

While opioid dependence is among the most severe and lethal of addictions, it also has the most effective medication treatments. The authors provide 2 case vignettes and a step-by-step process for clinical decision making.

The loss of control over urges and behaviors may be the central component of gambling disorders, but there is so much more to consider. Individuals with these problems have exponentially higher rates of suicide attempts and completions.
Is it possible to add creative twists to proven therapeutic techniques in order to encourage reluctant patients to try safe and effective treatments that we believe can benefit them? After reading the case, tell us what you think.
A 28-year-old married mother of 2 with a history of depression is brought to the emergency department after 6 months of near-daily methamphetamine use.

In clinical terms, one of the most distinguishing diagnostic features of addictive disorders is that those affected continually and repeatedly revert to their addictive behaviors, despite the devastating negative and adverse consequences.