
Test your knowledge on traumatic brain injuries (TBI) and their resultant effects on cognitive function and mental health.

Test your knowledge on traumatic brain injuries (TBI) and their resultant effects on cognitive function and mental health.

While some psychiatrists may doubt the connection between climate disruption and psychiatric disorders, the evidence is growing stronger every day.

Although it is still widely believed that the management of chronic pain usually requires medications or physical interventions, a growing body of research has demonstrated the efficacy of psychological therapeutic modalities.

Research published more than 25 years ago was already reporting problems with opioid analgesics.

A review of systemic medications for dermatologic diseases describes a wide range of adverse events, which range from mild and reversible to permanent and potentially fatal.

Take this quiz on one of the most controversial diagnoses in pain management.

Which gene is not associated with risk for the development of TD? What is the prevalence of TD in patients with schizophrenia treated with antipsychotics? Those questions and more in this quiz.
Because over half of persons with HIV infection have a lifetime history of depression or bipolar disorder, psychiatrists are uniquely positioned to provide both preventive and therapeutic interventions to vulnerable patients.

Could right-to-die laws result in people requesting death, even in the face of of potentially treatable health problems?
A report on substance abuse and HIV research around the world.
Whether marijuana use should be legalized is a subject worthy for debate. It is unfair, however, for patients who have real health problems to be misled into believing that there is a magical cure.
Renal failure is not an uncommon disorder either in the general public or in patients with psychiatric disorders, but accompanying depression, anxiety, and loss must be attended to during such an illness.

Psoriasis, a chronic inflammatory, autoimmune skin disorder, is associated with both genetic and environmental factors. It has important treatment implications for patients who have psychiatric disorders.

There are probably few health care professionals who are unaware of the concerns about the apparent overprescription of opioids. However, we have had only limited information on how good a job physicians may actually be doing in prescribing these medications.

Psychiatrists should be playing a key role in end-of-life decisions as well as, not coincidentally, in pain management.


Migraine, particularly chronic migraine, as well as other chronic headaches, have high rates of comorbidity with mood and anxiety disorders.

In addition to their use in the management of epilepsy, anticonvulsants are indicated for management of bipolar disorder, mania, neuralgia, migraine, and neuropathic pain.

While tremendous therapeutic advancements have been made, patients with rheumatoid arthritis (RA) have a myriad of comorbidities, including fatigue, depression, and sleep disturbances. Data on the comorbidity of psychiatric disorders with arthritis are also striking: according to the NIMH Catchment Area program, the lifetime prevalence of psychiatric disorders among patients with RA is 63%.

neurotoxins, glatiramer acetate, organophosphate exposure, glioma, glioblastoma, lipoprotein-associated phospholipase A2 (Lp-PLA2), C-reactive protein (CRP), stroke, neurorehabilitation, trigeminal neuralgia
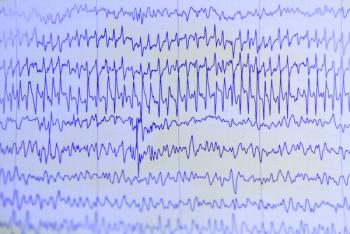
Affected patients with intractable epilepsy are treated, often for years, with antiepileptic drugs and other interventions that can promote further morbidity.