
How targeted interventions may reduce the burden of premature mortality among patients with schizophrenia and other psychiatric disorders.


How targeted interventions may reduce the burden of premature mortality among patients with schizophrenia and other psychiatric disorders.

This issue of Psychiatric Times covered government fraud, emergency psychiatry, PTSD in practicing psychiatrists, college mental health, and other critical issues.

Nearly half of children who present to emergency departments with self-harm receive no mental health assessment. What are the essential elements needed to interview children and adolescents in the context of a psychiatric emergency?

Jails have a much higher percentage of homeless mentally ill than does the general community, and those with psychiatric disorders (eg, schizophrenia) must often fend for themselves. Here are some solutions.

Currently, 1 in 15 youths undergoing psychiatric evaluation in the emergency department is restrained. This article covers diagnostic and therapeutic interventions that can reduce fear and put the young patient on a path to recovery.
It is important to recognize and document the abilities and deficits of a patient in order to determine capacity.

Acute intoxication is the most likely culprit for an increased risk of violence or agitation, but personality, psychosis, and cognitive problems can all play a role. A skilled clinician can glean a great deal of information in a short period of time.

There is an impressive array of presentations and speakers at an upcoming meeting, the only one in the country to address behavioral emergencies in the acute care setting.

There has probably never been a worse place and worse time to have a severe mental illness than now in the United States. How did we get into this mess?
Good documentation can be used by psychiatrists to enhance the physician-patient relationship. Of course, transparency could come at a price to practitioners, so following reasonable guidelines outlined in this article is key.

Many years ago, the model approach to mental health treatment was the therapeutic community: "As Aristotle noted long ago, man is a social animal and only in a social unit can he experience a whole life." More in this blog.

In the US, suicide is a leading cause of death, ranking third among youths aged 15 to 24. Rates of suicide attempts and death are highest among US Pacific Island indigenous youths. Emergency departments play a key role in suicide prevention, especially in this and other minority populations.

A video summarizing key points of a presentation titled “Agitation and Aggression: Managing the Acute Episode and Beyond, An Evidence-Based Approach.”
Agitation is a spectrum of symptoms . . . it can go all the way from being irritable up to pacing to lashing out to clenched fists to outright violence. Intervention via de-escalation techniques at an early stage is optimal. More in this podcast.

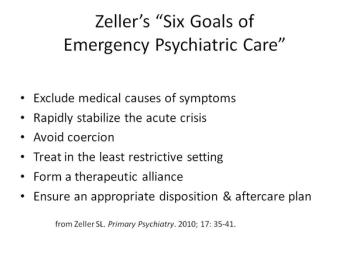
Emergency psychiatry is helping to redefine acute mental health treatment-facilitating timely access, in less restrictive, outpatient levels of care, for patients in crisis.

In the eyes of many, the current societal approach to the treatment of psychiatric disorders cannot possibly be considered humane. More in this commentary.

Psychiatrists are urged to familiarize themselves with these new drugs and the typical presentations of patients who use them since implications of misdiagnosis can be far-reaching.

Ideology is much less important than common sense solutions. The mentally ill have many unmet needs and suffer from great and undeserved coercion.

Emergency departments are often forced to hold patients who are acutely dangerous to themselves or others for long periods until an inpatient bed can be obtained.

This article highlights several features of medical and social importance that are somewhat unique to the Somali refugee community in the US.

A resident describes her experience in dealing with a potentially agitated patient.

A therapeutic alliance can serve to build a trusting relationship between clinician and patient and increase the patient’s feelings of agency and autonomy.

For now, it is encouraging to know that psychiatrists remember that they, too, are physicians first who can tap into their medical training to provide comprehensive patient care.

The rise in suicides and lethal overdoses of opioid analgesics is probably not coincidental. In most overdose deaths, we have no way of knowing with any degree of certainty whether they were accidental deaths or intentional suicides.

Both clinicians and weather forecasters employ the same general process of information gathering, analysis, and reaching a conclusion.