Methods of identifying and understanding the intricacies of psychosis in clinical settings.
Methods of identifying and understanding the intricacies of psychosis in clinical settings.

For patients suffering the chronic, debilitating symptoms of schizophrenia, antipsychotic medication is a critical component of treatment-and may literally be life-saving.

How to make cognitive behavioral therapy for psychosis feasible in a busy practice with limited resources.

The key to identification of prodromal psychosis may lie in community-based outreach.
The personalized medicine approach is predicated upon a greater understanding of the biology of illness and how it plays out-uniquely and specifically-for each individual patient.

First-episode psychosis cases are presented here using the RAISE study model-individual sessions, family psycho-education, social advancement in school work, and an expert psychiatrist prescriber.

Is clozapine still the gold standard for treatment-resistant schizophrenia?

Do atypical antipsychotics increase the risk of major malformations among exposed infants?
Check out what's new in schizophrenia research, personality disorders, patient education, integrative psychiatry, addiction, and more.

For too long the treatment needs of the seriously mentally ill have been ignored by SAMSHA, and this needs to change, says this psychiatrist.

Both the literature and clinical experience point to considerable risk in discontinuing antipsychotic treatment, for many chronically psychotic patients. Here's why.
Editors' choices of noteworthy psychiatry stories from around the Web: genetics of schizophrenia, Alzheimer disease, the perils of mixing prescription and over-the-counter medications, new guidelines for treating pain with opioids, and other topics.

Reasons for the overall low rate of clozapine use brings to light questionable decisions on the part of policymakers

For a change, here is some very good news coming from several fronts. "It’s almost like science fiction, but it’s real."
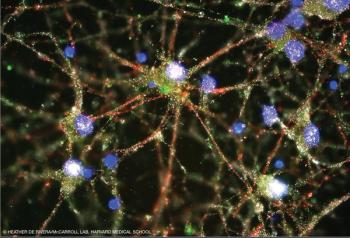
The identification of a genetic risk factor has shed light on the underlying neurobiology of the disorder.
Groundbreaking work by a Harvard team represents a bold step in our journey toward understanding schizophrenia.

A simple handshake is no longer a formal gesture to symbolize parting ways. It has become that moment, with a patient, when we both agree to embark on a journey together.
Setting the record straight on what the literature does and does not say about long-term use of antipsychotics.

Brain-based biomarkers identify more biologically homogeneous categories of psychosis than do clinical diagnoses.

Are you up-to-date on the risk of recurrent pneumonia in patients with schizophrenia when an antipsychotic is reintroduced?
Editors' picks, including the biggest story of the year thus far and others of interest to psychiatrists and the public.

New evidence-coupled with advances in molecular biology-has afforded an unparalleled opportunity to move toward identifying potential new treatments for schizophrenia.

A report of initiatives that have raised awareness of and promoted data sharing and data transparency in order to advance science and improve public health and health care.

Neuroinflammation may be a culprit in the development of psychosis. What are the clinical implications?

How targeted interventions may reduce the burden of premature mortality among patients with schizophrenia and other psychiatric disorders.