
How can we keep the public safe and reopen the economy at the same time?

How can we keep the public safe and reopen the economy at the same time?
The next several years will present challenges and opportunities for psycho-oncology to improve care for patients.

There are myriad nuanced clinical approaches to cancer treatment, and psychosocial factors are no less complex.

An added component of cancer treatment is discovering what is most meaningful in the patient’s life and using that to buoy them during difficult moments. That, in a nutshell, is the psychiatrist's role.
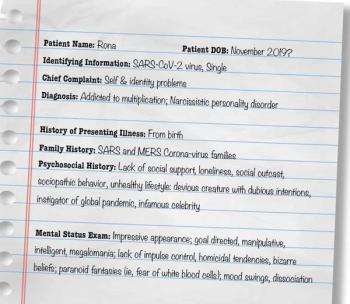
British researchers find neuropsychiatric complications associated with COVID-19.

A nationwide cohort study sought to determine the clinical course of schizophrenia in women and men in order to improve diagnostic accuracy and design guidelines.

The role of neuroimaging is to rule out medically or surgically treatable causes of illness, such as new-onset psychosis.

You are cordially invited to submit an article about a “what if” legal dilemma for a series about psychiatry and the law.

Psychiatry has changed, and we now have an acute awareness of the cost of sexual trauma to patients. When it comes to race, however, we still have a lot to learn.

A position paper presents the best ways to use electronic communication, particularly timely given the pandemic.
One can only hope today's challenges will become a “corrective emotional experience."

This moment in history cannot be lost. When you ask us if we are okay, be prepared to hear us say we are not . . . and never have been. Then be prepared to do more.

Women should be provided with multiple options for treatment if they decide to engage in mental health care during this critical period.

When the patient has significant comorbid psychiatric problems, high risk of suicide, and Huntington disease, the role of clinician spills over into patient advocate in a complex medical system.

At one time, most medical school classes took the Hippocratic oath, but that is no longer the case.

It is much easier to treat depression after 6 months of non-response than 6 years, regardless of which intervention is used, so time is of the essence.

In this interview, Dr Aftab and Dr Johnstone discuss her criticisms of psychiatric diagnosis and her approach to psychological formulation as a conceptual alternative to diagnosis.

What can be done about racism? We're so glad you asked.

A synthetic derivate of the endogenous amino acid L-cysteine and a precursor of glutathion, N-Acetylcysteine shows promise for treating a variety of psychiatric disorders.

There are some off-label proposed uses for topiramate in comorbidities that are common in patients with bipolar disorder. What does the evidence say?

Wake up, arise from the fog, and face a new post-op day.

The medical community must examine how and what we can do to welcome and serve the black and brown communities that may view us as the authority they dare not call.

Psychiatrists should be experts at hearing and seeing what is not visible. That is exactly what we need to do to let the sun shine through the racist dust.

Reflections on the current psychiatric literature as well as the many accomplishments psychiatry has seen since the 1950s.

Clinical considerations for evaluating treatment options for patients with insomnia and AUD versus patients with primary insomnia without substance use comorbidity.

With everything going on in the world, this lesson has become abundantly clear—our attitudes will help us ride the ups and downs and the slings and arrows that present themselves and propel us to better times.

Inevitably, some of your patients will need of emergency psychiatric services. These tips will help prepare you and your patients when a crisis unfolds.

Sometimes our best intentions lead us down the wrong road. By reconsidering a few seemingly harmless questions, this psychiatrist was able to make the most of his medication-check visits with his patients.

New data and an intriguing case example suggest the mortality rate may be decreasing. What does this mean for the days ahead?

A case of a patient with difficult-to-treat insomnia highlights the pervasive daytime effects of this condition.